Overview
Comprehensive Vascular Solutions with Precision Care at Aster CMI
Minimally Invasive Treatments. Complex Surgeries. All Under One Roof.
Aster CMI Hospital in Bangalore is a premier destination for ultra-modern vascular and endovascular treatment. From simple vein conditions to high-risk arterial disorders, our expert team delivers comprehensive care using contemporary technology in a dedicated hybrid vascular suite.
Our vascular and endovascular surgeons bring decades of experience and global training, delivering precise, customized care—even in the most challenging, high-risk cases.
Integrated care from a multidisciplinary team—vascular surgeons, interventional radiologists, cardiologists, nephrologists, and rehab specialists—for better outcomes and faster recovery.
Equipped with advanced imaging, catheter-based tools, and surgical capabilities in one setting—enabling faster, safer, and minimally invasive interventions.
Consistently high success rates in treating complex vascular conditions and emergencies, backed by clinical excellence, innovation, and patient-first protocols.
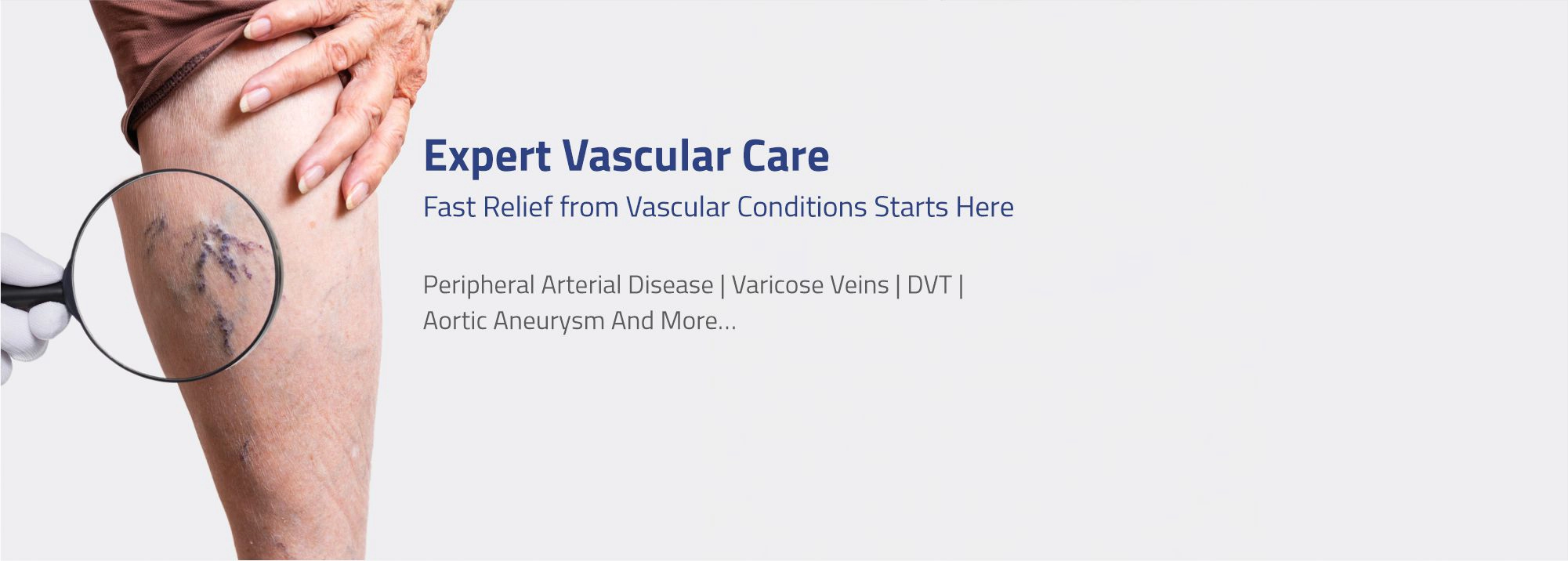
Conditions We Treat
At Aster CMI Bangalore, our vascular specialists treat a wide range of conditions affecting arteries, veins, and circulation with advanced, personalized care.
- Peripheral Artery Disease (PAD)
- Aortic Aneurysms
- Carotid Artery Disease
- Varicose & Spider Veins
- Deep Vein Thrombosis (DVT)
- Renal & Mesenteric Ischemia
- Vascular Trauma & Emergencies
- Thoracic Outlet Syndrome
- Chronic Venous Insufficiency
- Raynaud’s Disease, Buerger’s Disease
Treatments & Procedures Offered
A combination of conventional and minimally invasive treatments is provided, carefully chosen to meet the needs and conditions of each patient.
- EVAR (Endovascular Aneurysm Repair)
- Peripheral Angioplasty & Stenting
- Carotid Endarterectomy & Stenting
- Laser & Radiofrequency Vein Treatments
- AV Fistula & Vascular Access Surgery
- Sclerotherapy for Varicose Veins
- Thrombolysis & DVT Management
- Aortic & Bypass Surgeries
- IVC Filter Placement & Retrieval
- Limb Salvage & Trauma Repair
Technology That Sets Us Apart
- Hybrid Vascular Suite: Precision imaging + surgical intervention in one setting.
- High-Resolution Diagnostics: Vascular ultrasound, CT angiography, and MR angiography.
- Advanced Laser and Radiofrequency Tools: Designed for precision treatment with minimal discomfort and faster recovery times
Our expert teams are committed to delivering evidence‑based, family-centred care in every subspecialty.
Get in Touch
Aster CMI Hospital, Hebbal, Bangalore
Find the right vascular specialist near you and take control of your vascular health today.
Ready to take the next step? Book your appointment or connect with our care team today—your vascular health starts here.
Vascular surgery is a specialized medical field dedicated to diagnosing and treating conditions affecting the body's blood vessels, including arteries and veins. Surgeons in this field address various issues such as arterial blockages, aneurysms, and venous insufficiencies (Varicose veins & DVT). Procedures involve repairing, removing, or rerouting vessels to restore proper blood flow, prevent potential complications like strokes or tissue damage, and alleviate symptoms such as pain or swelling. By managing vascular health, vascular surgeons play a crucial role in enhancing circulation, preserving limb function, and ultimately improving the overall well-being of their patients.
To determine the necessity for vascular surgery procedures, a vascular surgeon may carry out various diagnostic tests to assess the blood flow and determine the need for a procuedure or may even prescribe medications with suggestions for lifestyle mobification. However, symptoms of vascular disease caused by blood clots may not become apparent until the clot grows significantly large enough to obstruct blood flow.
Percutaneous (performed through the skin) transluminal interventions are used to treat both acute and chronic peripheral vascular disease (PVD). These interventions encompass procedures such as angioplasty, stenting, and atherectomy. In comparison to surgical methods, percutaneous techniques often present advantages such as lower risk, speedier recovery, and greater cost-effectiveness.
It's important to note that aortic aneurysms can develop and grow without causing any noticeable symptoms. More often, they are detected incidentally during a CT scan or ultrasound scan for unrelated conditions. However, when the aneurysms grows large , they may present with some of the following symptoms.
Shortness of breath
Coughing
Chest or back pain
Difficulty breathing and swallowing
Throbbing sensation near the navel
Deep abdominal pain on the side
Feeling a pulsating sensation near the navel or in the abdomen.
Feeling unwell in the stomach or experiencing vomiting, sweating, and dizziness if the aneurysm ruptures
Treatment options for aortic aneurysms depend on factors like the size, location, and overall health of the patient. The main approaches include:
1. Monitoring: Small aneurysms that are not causing symptoms may be monitored regularly through imaging tests to track their size and growth rate.
2. Medication: Medications to control blood pressure and cholesterol might be prescribed to manage risk factors that contribute to aneurysm growth.
3. Open Surgery: In cases where the aneurysm is large or at risk of rupture, open surgical repair involves replacing the weakened portion of the aorta with a synthetic graft.
4. Endovascular Aneurysm Repair (EVAR/TEVAR/FEVAR/ChEVAR): This minimally invasive procedure involves inserting a stent graft through small incisions in the groin, threading it to the site of the aneurysm, and positioning it to reinforce the weakened aorta wall.
5. Hybrid Procedures: Sometimes a combination of open surgery and endovascular techniques is used for complex cases.
6. Emergency Repair: If an aneurysm ruptures, emergency surgery is required to repair the rupture and prevent life-threatening internal bleeding.
The choice of treatment depends on the aneurysm's characteristics and the patient's overall health. Early detection, regular check-ups, and discussions with vascular specialists are crucial in determining the best course of action.
Peripheral Arterial Disease (PAD) is a circulatory disorder characterized by narrowed or blocked arteries, commonly in the legs. It's caused by atherosclerosis, where plaque buildup restricts blood flow, leading to reduced oxygen supply to muscles and tissues. Symptoms include leg pain, cramping, or fatigue during physical activity (claudication), and in severe cases, even at rest. PAD increases the risk of complications like non-healing ulcers, infections, and even limb amputation. Lifestyle changes, medication, exercise, and in some cases, surgical interventions are used to manage PAD, improve blood circulation, and mitigate its impact on overall cardiovascular health.
Treatment options for Peripheral Arterial Disease (PAD) include lifestyle changes, medications, and medical procedures:
1. Lifestyle Changes: Quitting smoking, adopting a healthy diet, regular exercise, and managing diabetes and high blood pressure can improve blood flow and symptoms.
2. Medications: Antiplatelet drugs (aspirin, clopidogrel), cholesterol-lowering medications (statins), and medications to control blood pressure and manage symptoms (cilostazol) are commonly prescribed.
3. Exercise Therapy: Supervised exercise programs help improve walking distance and reduce symptoms.
4. Angioplasty and Stenting: Minimally invasive procedures involving balloon angioplasty and stent placement to open narrowed arteries and improve blood flow.
5. Bypass Surgery: Surgical creation of a new path for blood flow using a graft to bypass blocked arteries.
6. Thrombolytic Therapy: Medications used to dissolve blood clots in cases of acute limb ischemia.
7. Wound Care: Specialized wound care is crucial for healing non-healing ulcers and preventing infections.
8. Smoking Cessation: Quitting smoking is essential to improve blood circulation and overall health.
The treatment plan depends on the severity of PAD and individual patient factors. A vascular surgeon will assess the condition and recommend the most appropriate approach, often combining multiple methods to achieve the best outcomes.
Vascular surgeons treat a wide range of conditions related to blood vessels, both arteries and veins. These include:
1. Arterial diseases: Blockages (atherosclerosis), aneurysms, and dissections in arteries, often in the legs (peripheral arterial disease) or the aorta.
2. Venous diseases: Varicose veins, deep vein thrombosis (DVT), and chronic venous insufficiency.
3. Aortic conditions: Aneurysms (abnormal enlargements) in the aorta, the body's main artery.
4. Carotid artery disease: Blockages or narrowing in the carotid arteries, which supply blood to the brain.
5. Renal and mesenteric artery disease: Blockages affecting arteries that supply blood to the kidneys and intestines.
6. Hemodialysis access: Creating and maintaining access points for patients requiring hemodialysis treatment.
7. Trauma: Treating vascular injuries caused by accidents or trauma.
8. Diabetic foot problems: Addressing circulation issues and wounds in patients with diabetes.
9. Vascular malformations: Managing congenital or acquired vascular abnormalities.
Vascular surgeons perform various procedures, such as angioplasty, stent placement, bypass surgery, endarterectomy, and thrombectomy, to treat these conditions and ensure proper blood flow and vascular health.
Risk factors linked to all major vascular conditions include:
Diabetes
Hyperlipidemia (increased levels of fats in the blood, like cholesterol and triglycerides)
Smoking
High blood pressure
Obesity
Lack of physical activity
Dietary preferences
Family history
Pregnancy
While it's essential to understand that these risk factors amplify the likelihood of disease development, however, they do not necessarily act as direct causative factors. Some individuals with one or multiple risk factors may never experience the disease, while others without any known risk factors might still develop the condition.
Aortic aneurysm is a condition characterized by the abnormal enlargement of the aorta, the primary blood vessel that carries blood throughout the body. This ballooning expansion of the aorta gradually increases in size over time.
Both aortic aneurysm and dissection are critical medical conditions. Aortic aneurysm rupture ranks among the leading global causes of mortality, with 50% of patients succumbing to the condition before reaching medical care facilities.
At Aster CMI Hospital, the following tests are used to detect the presence of an aortic aneurysm -
CT Aortogram
X-ray
Ultrasound scan
MR Aortogram
Conventional Angiogram
In the event of an aneurysm rupture, immediate surgical intervention becomes necessary.
For individuals with weakened blood vessels in the chest and abdomen regions, a procedure known as endovascular stent graft surgery is employed. This minimally invasive surgical technique aims to reinforce and repair compromised blood vessels.
Peripheral Arterial Disease (PAD) can cause a variety of symptoms, primarily due to reduced blood flow to the legs and feet. Common symptoms include:
1. Claudication: Pain, cramping, or aching in the legs during physical activity, which typically subsides with rest. The pain is often felt in the calf muscles.
2. Leg Weakness or Numbness: A feeling of weakness or numbness in the legs, particularly during walking or other forms of exercise.
3. Cold Extremities: The legs and feet might feel colder than the rest of the body, and the skin may appear pale or bluish.
4. Slow Healing Wounds: Wounds, cuts, or sores on the feet or legs that heal slowly or don't heal at all.
5. Gangrene: In severe cases, reduced blood flow can lead to tissue death (gangrene), causing blackened, non-healing wounds or areas of skin.
6. hair Loss and Skin Changes: Reduced blood supply can result in thinning or loss of hair on the legs, as well as changes in the texture and color of the skin.
7. Weak Pulses: Weakened or absent pulses in the feet or legs when checked by a healthcare professional.
It's important to note that some individuals with PAD might not experience noticeable symptoms, especially in the early stages. If you suspect you might have PAD or experience any of these symptoms, it's advisable to seek medical evaluation, as early detection and management can help prevent complications and improve overall quality of life.
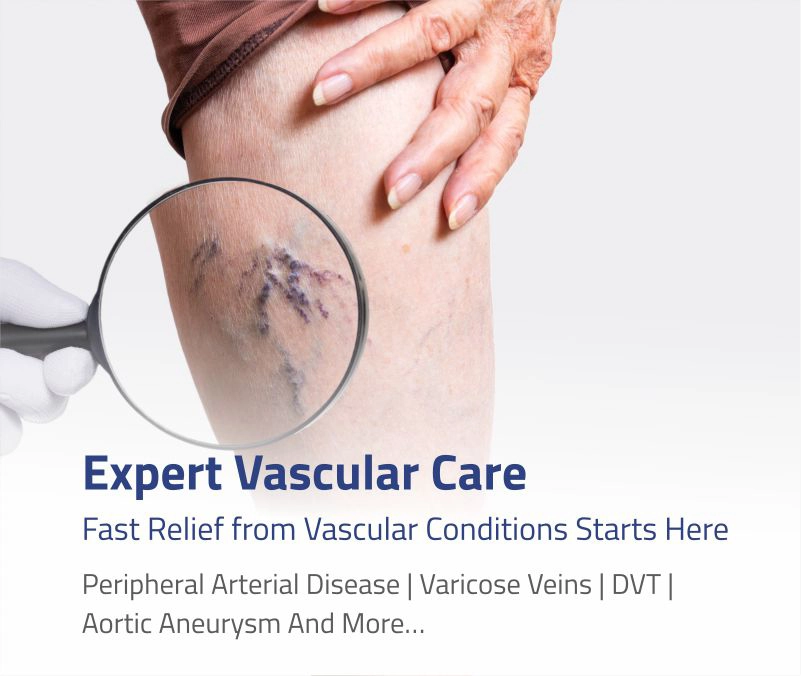
Varicose veins are swollen, twisted veins that often appear dark blue or purple on the skin's surface. Common symptoms of varicose veins include:
1. Visible Bulging Veins: Twisted, enlarged veins that are visible just under the surface of the skin, often resembling cords or ropes.
2. Aching or Pain: Aching, throbbing, or burning sensations in the legs, especially after standing or sitting for extended periods.
3. Heaviness or Fatigue: A sense of heaviness, fatigue, or discomfort in the legs, particularly towards the end of the day.
4. Swelling: Swelling, especially around the ankles and lower legs.
5. Itching or Irritation: Skin over varicose veins might become itchy or irritated.
6. Cramping: Muscle cramps or spasms in the legs, particularly at night.
7. Skin Changes: Skin around the affected area might become discolored, dry, or inflamed.
8. Ulcers: In severe cases, varicose veins can lead to skin ulcers near the ankles, which are difficult to heal.
It's important to note that not all varicose veins cause symptoms, and the severity of symptoms can vary. If you're experiencing discomfort or are concerned about varicose veins, it's advisable to consult a vascular surgeon for evaluation and appropriate management.