Neurology is a branch of medicine concerned with the study and treatment of disorders related to the nervous system. The Neurology department at Aster CMI Hospital is one of the best neurology hospitals in Bangalore. We provide evidence-based treatments for a variety of neurological conditions, such as stroke, Alzheimer’s disease, Parkinson’s disease, epilepsy and movement disorders.
We have the best neurologists in Bangalore, who are well acquainted with the latest developments in the field of neurology. Our neurologists are also supported by trained nurses, rehabilitation therapists, and other clinicians who ensure that our patients have an all-around treatment and faster recovery.
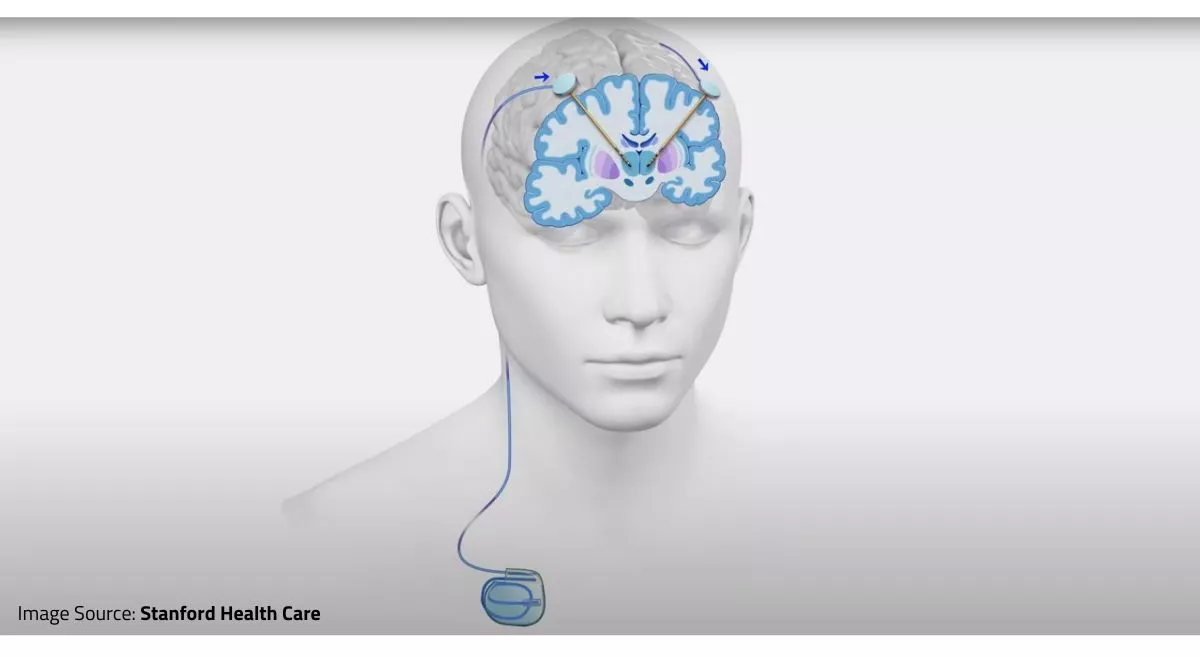
The department of neurology is well-equipped with the latest infrastructure and technology which are required for the diagnosis and management of neurological conditions.
Aster NeuKIDS
Aster CMI is proud to present its latest speciality: neurological sciences and treatment just for children. Our brand new department, which will be a subset of our award-winning neuroscience discipline, will provide attenuated neurology care—from diagnosing and treating common conditions such as headaches to conditions like epilepsy, newborn developmental delay and learning issues in teenagers.
In addition, Aster NeuKIDS also provides these facilities:
Management of difficult epilepsy in children of all ages
Specialised PICU and paediatric neurosurgery support
Well-equipped child development centre that helps generate the best outcome for children with neurological issues
Trained dieticians to support and educate guardians about children with epilepsy on ketogenic diet
Our Doctors
We have some of the best specialists from around the world, they bring years of experience and offer evidence-based treatment to ensure the best care for you.
Treatments & Procedures
We provide comprehensive treatment for all types diseases under one roof. Our highly experienced doctors supported by especially trained clinical staff, ensure the best care for you.
Advanced Technology & Facilities
Well equipped with the latest medical equipment, modern technology & infrastructure, Aster Hospital is one of the best hospitals in India.
Patient Stories
Our patients are our best advocates, hear the inspiring stories of their treatment journey
Blogs
The source of trustworthy health and medical information. Through this section, we provide research-based health information, and all that is happening in Aster Hospital.