Introduction
Parkinson’s disease (PD) is a chronic neurodegenerative disorder that primarily affects movement. With symptoms of tremor, rigidity, bradykinesia (slowness of movement), and postural instability, Parkinson's has a considerable bearing on the quality of life of a patient. While there is no cure for PD, multiple therapeutic options are offered to treat its symptoms. One of the most advanced and effective treatment therapies is Deep Brain Stimulation (DBS).
DBS has revolutionized the Parkinson's treatment scene, offering symptom relief to those patients who fail to respond effectively to medication anymore. This blog discusses DBS, its action, efficacy, advantages, risks, and inclusion criteria, and how it is affecting the treatment of Parkinson's disease. Since we are marking World Parkinson's Day on April 11 and Parkinson's Awareness Month during the entire month of April, we must create awareness about developments like DBS, which greatly improve the lives of individuals suffering from this intense disease. If you are looking for expert care, choosing a reputed Neurology Hospital in Bangalore can ensure access to the latest therapies and specialized treatment.
What is Deep Brain Stimulation (DBS)?
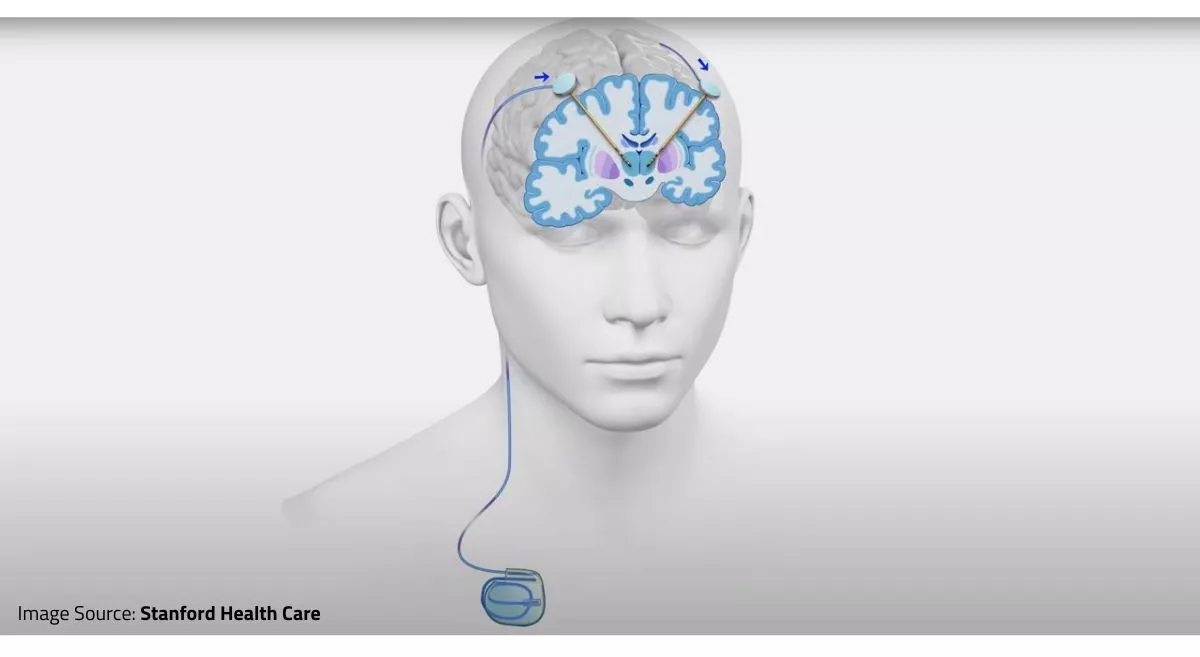
Deep Brain Stimulation (DBS) is a neurosurgical operation where a tiny device is implanted in the brain to provide electrical impulses to certain areas. It is similar to a pacemaker for the brain, regulating abnormal neural activity responsible for movement disorders. The device has three principal parts:
- Electrodes: Implanted in specific brain areas like the subthalamic nucleus (STN) or globus pallidus interna (GPi).
- Implantable Pulse Generator (IPG): A battery-powered device that is implanted just below the skin near the chest.
- Extension Wire: Connects the electrodes to the pulse generator.
After being implanted, the DBS device delivers controlled electrical impulses to modulate the abnormal brain activity that causes Parkinson's symptoms. This modulation relieves movement-related problems, enabling patients to regain some control over their motor functions.
How DBS Helps in Parkinson's Disease?
Parkinson's disease is linked with the loss of dopamine-producing neurons in the brain, specifically in the substantia nigra. This disrupts communication between brain areas, resulting in motor symptoms. DBS does not replace dopamine but assists in modulating abnormal neural circuits and diminishing excessive or lacking signaling.
DBS focuses on certain specific regions of the brain:
- Subthalamic Nucleus (STN): Stimulation here reduces tremors, rigidity, and bradykinesia.
- Globus Pallidus Interna (GPi): Stimulating this area enhances dyskinesia (movement) and dystonia.
- Thalamus (Ventral Intermediate Nucleus – VIM): Used mostly to control tremors.
By controlling these areas, DBS enhances motor function and diminishes the requirement for excessive medication dosages, resulting in fewer side effects. Moreover, certain research has indicated that DBS could have benefits outside of motor functions as well, such as lessening depression and enhancing sleep habits among Parkinson's patients.
The DBS Procedure: Step-by-Step Explanation
DBS surgery is typically done in two stages:
- Electrode Placement
- The patient remains awake during this step to provide immediate feedback.
- A neurosurgeon drills small holes in the skull to implant thin electrodes in the targeted brain area.
- Electrical impulses are tested to ensure optimal relief from the symptom.
- Once the correct positioning is determined, the electrodes are fixed.
- Pulse Generator Implantation
- A small device (IPG) is inserted under the skin close to the chest.
- The equipment is attached to the electrodes through extension leads.
- Once the healing is complete, the equipment is programmed externally so as to provide the appropriate amount of stimulation.
- Follow-up visits are necessary to reprogram the settings according to the patient's response.
The whole process takes a few hours, generally, and recovery time is variable. Following the surgery, monitoring is critical to adjust the levels of stimulation to get optimum benefits.
Advantages of DBS in Parkinson’s Patients
DBS has several advantages, which make it one of the best treatments for advanced Parkinson's disease:
- Improved Motor Symptoms: Tremors, stiffness, and slow movement are greatly reduced.
- Less Dependence on Medication: Patients can take smaller doses of Parkinson's medication, which minimizes side effects such as dyskinesia and nausea.
- Better Quality of Life: DBS enables patients to recover their independence in daily activities.
- Long-Term Effects: In contrast to medications that lose their effect, DBS delivers ongoing symptom relief.
- Customizable Settings: The stimulation can be fine-tuned as required, providing tailored treatment.
- Potential Cognitive and Emotional Advantages: Some patients experience improved mood and sleep quality.
Are there any Risks and Side Effects of DBS?
Although DBS is safe, it does have some risks:
- Surgical Risks: Infection, bleeding, stroke, or brain swelling can occur in some cases.
- Device Malfunction: Hardware issues may necessitate additional surgery.
- Cognitive and Psychological Effects: Mood changes, depression, or memory problems can be experienced by some patients.
- Speech and Balance Issues: Speech slurring and balance problems may arise in a few cases.
- Battery Replacement: The battery of the device may need replacement after a few years with a simple procedure.
Who is an Ideal Candidate for DBS?
Not all Parkinson’s patients are suitable candidates for DBS. Physicians look at the following factors before suggesting DBS:
- Advanced Parkinson’s Disease: Patients with prominent motor symptoms that cannot be controlled well with medication.
- Response to Levodopa: If Levodopa causes relief from symptoms, DBS is expected to be helpful.
- Lack of Severe Cognitive Decline: Patients suffering from dementia or severe memory impairment are generally not good candidates for DBS.
- No Major Psychiatric Disorders: Anxiety or severe depression can be worsened by DBS, and thus, patients having those conditions should be avoided.
- Good Overall Health: Patients need to be in good overall health to withstand the surgery and recovery process.
DBS vs. Medication Therapy
The majority of Parkinson's patients begin with medication therapy, including Levodopa, dopamine agonists, and MAO-B inhibitors. Medications are effective in the initial stages but, with long-term use, tend to cause fluctuating responses and dyskinesia. DBS offers more stable symptom control without the "on-off" phenomenon associated with medication therapy. DBS does not, however, eliminate medications completely, but decreases reliance on them.
Future of DBS and Advancements
Continued research is refining DBS to make it even more useful for Parkinson's treatment. Breakthroughs include:
- Adaptive DBS (aDBS): Continuously adjusts stimulation in real time according to brain activity.
- Non-Invasive DBS: Researching ways to provide stimulation without surgery.
- DBS with Neurofeedback: Employing AI and machine learning to fine-tune therapy.
- Gene Therapy and Stem Cells: Potential future therapies that may supplement DBS.
Conclusion
As we mark Parkinson's Awareness Month, it is essential to highlight the progress and advancements made in treating Parkinson's. Deep Brain Stimulation has transformed Parkinson's treatment, providing notable relief from motor symptoms and enhancing the quality of life for patients. It is not a cure but a long-term, tunable treatment for those who no longer fare well on medications. With ongoing technical advancements, DBS is increasingly effective, safer, and available. Patients contemplating DBS must meet with a Movement Disorders specialist or experienced Neurologists in Bangalore to find out if they qualify as candidates and to balance the benefits and risks. As more studies are conducted, DBS is poised to make Parkinson's disease care even better in the future.