The Department of Orthopaedics at Aster RV Hospital prides itself at providing world-class evidence-based treatment for a plethora of orthopaedic ailments. The department of orthopaedics is well equipped with a state of the art facility and is one of the leading quarterly centres in Karnataka .our experts are specialised in treating conditions related to the Hip, Knee, Shoulder, Hand, Spine, Paediatrics, Trauma, Foot and Sports Medicine they also pride themselves on the work done on regenerative orthopaedics.
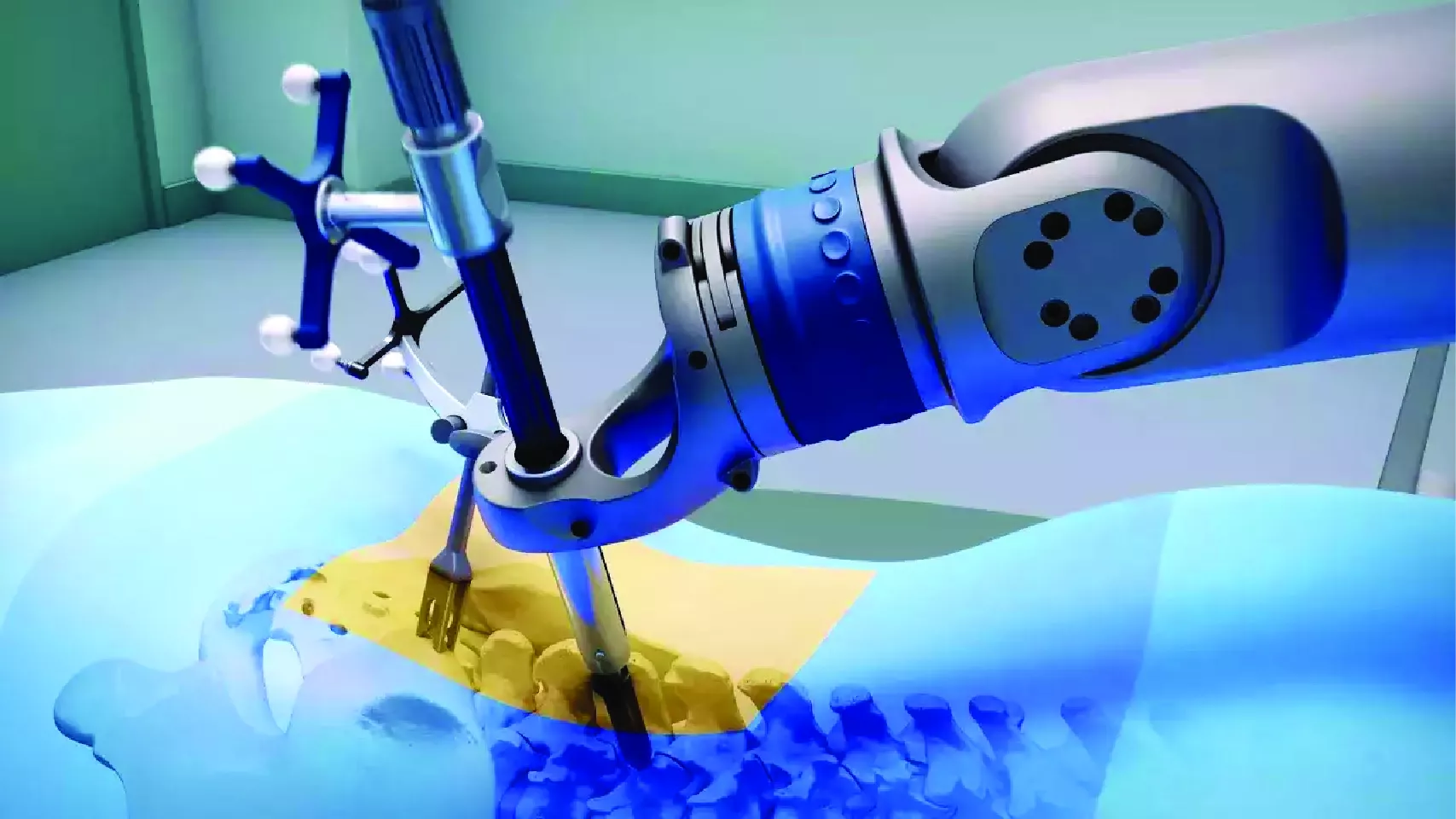
The unit performs complex precision surgeries which demand a high level of surgical skills and infrastructure delivering excellent outcomes which are patient-centric. The spectrum of surgical procedures performed ranges from primary arthroplasty to complex revision surgeries. Simple trauma to complex acetabular reconstructions. Polytrauma requiring a multidisciplinary approach and damage control orthopaedics.
The current decade marks the era of regenerative orthopaedics, the most promising treatment modalities of which are stem cells and PRP injections which provide treatment of early degenerative conditions which include early arthritis, avascular necrosis and other conditions like tennis elbow and plantar fasciitis.
This center of excellence houses advanced facilities including one of a kind fully equipped sports medicine unit. They are also supported by specially trained nurses, patient councillors and a state of the art physical rehabilitation centre. Making Aster RV one of the best orthopaedic hospital in J.P Nagar, Bangalore.
Our Doctors
We have some of the best specialists from around the world, they bring years of experience and offer evidence-based treatment to ensure the best care for you.
Advanced Technology & Facilities
Well equipped with the latest medical equipment, modern technology & infrastructure, Aster Hospital is one of the best hospitals in India.
FAQs
Want to find out more about the treatment? The answer to your questions can be found below.
When should a joint be replaced?
Moderate to severe arthritis interfering with daily activities.
What are the common causes of neglected fractures?
Neglected fractures can arise from various factors, including delayed medical attention due to lack of awareness, financial constraints preventing immediate treatment, or limited access to healthcare facilities. Patients may neglect seeking timely treatment for fractures for reasons such as underestimating the severity of the injury or lacking knowledge about available healthcare options.
How do you diagnose neglected fractures?
The diagnosis of neglected fractures involves a comprehensive approach. It includes a detailed patient history, thorough clinical examination, and imaging studies such as X-rays, CT scans, or MRI. The suspicion of a neglected fracture arises when there is evidence of delayed medical attention or signs of improper healing in the imaging studies.
Can neglected fractures be treated successfully, even after a delay?
Neglected fractures can be treated successfully, even with a delay in seeking medical attention. However, the success of the treatment depends on factors such as the type of fracture, the extent of the delay, and the overall health of the patient. While early intervention generally yields better results, late treatment can still provide significant benefits in many cases.
What is shoulder arthroscopy?
Shoulder arthroscopy is a minimally invasive surgical procedure that utilizes a specialized camera called an arthroscope and small instruments to diagnose and treat various shoulder conditions. It provides a detailed view inside the shoulder joint without the need for large incisions.
How is shoulder arthroscopy performed?
During shoulder arthroscopy, small incisions are made, and the arthroscope is inserted to visualize the shoulder joint. Specialized instruments are then used to repair or treat issues identified during the procedure. This minimally invasive approach reduces trauma to surrounding tissues.
What is the recovery time for shoulder arthroscopy?
Recovery time varies based on the specific procedure and individual patient factors. Generally, patients can expect a quicker recovery compared to open surgery. Early initiation of motion exercises and adherence to a rehabilitation plan are crucial for optimal recovery.
What is knee arthroscopy?
Knee arthroscopy is a minimally invasive surgical technique that employs a small camera and specialized instruments to diagnose and treat various knee conditions. It is commonly utilized for issues such as meniscal tears, ligament injuries, and cartilage damage.
How is knee arthroscopy performed?
Knee arthroscopy involves making small incisions through which an arthroscope is inserted to visualize the internal structures of the knee. Specialized instruments are then used to repair or remove damaged tissues, enabling a faster recovery compared to traditional open surgery.
What is the typical recovery period for knee arthroscopy?
Recovery duration varies based on the complexity of the procedure and individual factors. Generally, patients can resume normal activities within a few weeks, with physical therapy playing a crucial role in restoring knee function and strength.
Who is a candidate for hip replacement surgery?
Candidates for hip replacement surgery typically have severe hip pain, stiffness, and mobility limitations due to conditions such as osteoarthritis, rheumatoid arthritis, hip fractures, or avascular necrosis that have not responded to conservative treatments.
What is the recovery process like after hip replacement surgery?
The recovery process varies for each individual but typically involves a hospital stay of 1-3 days followed by physical therapy and rehabilitation to regain strength, mobility, and function in the hip joint. Most patients can resume normal activities within a few weeks to months after surgery.
How long does a hip replacement last?
The lifespan of a hip replacement implant varies depending on factors such as the patient's age, activity level, implant materials, and surgical technique. Generally, most hip replacements last 15-20 years or more before requiring revision surgery.
Will I need physical therapy after hip replacement surgery?
Yes, physical therapy is an essential part of the recovery process after hip replacement surgery. Physical therapists will work with patients to improve strength, flexibility, and range of motion in the hip joint, as well as teach proper techniques for walking and performing daily activities.
How can I prepare for hip replacement surgery?
Patients can prepare for hip replacement surgery by following their surgeon's preoperative instructions, which may include lifestyle modifications, medication adjustments, preoperative testing, and planning for postoperative care and rehabilitation. It's essential to communicate openly with the surgical team and address any concerns or questions before the procedure.
What is a multiligamentous knee injury?
A multiligamentous knee injury involves damage to two or more of the major ligaments in the knee, such as the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL).
These injuries often result from high-impact trauma, such as sports injuries, car accidents, or falls. They can involve direct blows to the knee or extreme twisting motions.
How is a multiligamentous knee injury diagnosed?
A comprehensive physical examination, along with imaging tests such as X-rays, MRI scans, or ultrasound, helps diagnose the extent of the injury and which ligaments are affected.
What is the recovery process like?
Recovery from a multiligamentous knee injury can be lengthy and requires patience and dedication to rehabilitation exercises. The timeline varies depending on the severity of the injury and the chosen treatment approach.
How can I prevent a multiligamentous knee injury?
Preventive measures include maintaining strength and flexibility in the muscles around the knee, using proper techniques during sports or physical activities, wearing appropriate protective gear, and avoiding risky movements or situations that could lead to injury.
How does a growth factor injection work?
The growth factors contained in the injection stimulate the body's natural healing processes, encouraging the repair of damaged cartilage, reducing inflammation, and potentially slowing down the progression of osteoarthritis.
Who is a suitable candidate for growth factor injection in the OA knee?
Patients with mild to moderate osteoarthritis of the knee who have not responded adequately to conservative treatments such as physical therapy, medication, and corticosteroid injections may be candidates for growth factor injections.
What are the potential benefits of growth factor injection for OA knee?
Benefits may include reduced pain, improved function and mobility, decreased inflammation, and potential regeneration of damaged cartilage, leading to long-term relief and improved quality of life.
What is a neglected fracture?
A neglected fracture is a type of bone break that has not received timely or appropriate medical treatment, resulting in delayed or insufficient healing. This delay often leads to complications and poses challenges in the management of the fracture, potentially affecting the overall outcome of treatment.
What are the potential complications of neglected fractures?
Complications associated with neglected fractures encompass a range of issues. These may include malunion, where the fractured bone heals in an improper alignment; non-union, indicating a failure of the bone to heal; deformities that affect the shape or structure of the bone; chronic pain; limited joint motion; and an increased risk of infection due to the prolonged exposure of the fracture site.
What treatment options are available for neglected fractures?
The treatment of neglected fractures is individualized based on the specific characteristics of the fracture. Surgical intervention may be required, involving procedures such as fracture reduction, fixation using implants, or bone grafting. Physical therapy and rehabilitation play a crucial role in restoring functionality, and the treatment plan may be more complex than for fractures addressed promptly.
What challenges may arise in the treatment of neglected fractures?
Addressing neglected fractures poses unique challenges. These challenges may include correcting bone deformities resulting from delayed treatment, managing complications such as infections that may have developed over time, and achieving stable fixation during surgical procedures. Additionally, the rehabilitation process may be more prolonged, and patients may require additional support and monitoring.
What conditions can be treated with shoulder arthroscopy?
Shoulder arthroscopy is versatile and can address conditions such as rotator cuff tears, labral tears, shoulder impingement, frozen shoulder, and recurrent dislocations. Its dual diagnostic and therapeutic capabilities make it a valuable tool for orthopedic surgeons.
What are the benefits of shoulder arthroscopy over traditional open surgery?
Shoulder arthroscopy offers several advantages, including smaller incisions, reduced damage to surrounding tissues, faster recovery times, and decreased postoperative pain. Patients often experience improved range of motion and function with this less invasive approach.
Are there risks associated with shoulder arthroscopy?
While shoulder arthroscopy is considered safe, potential risks include infection, bleeding, nerve injury, or stiffness. However, the overall complication rate is relatively low, and the benefits of the procedure often outweigh the risks.
What knee conditions can be addressed with arthroscopy?
Knee arthroscopy is suitable for treating a range of conditions, including meniscal tears, ligament injuries like ACL tears, cartilage damage, and synovitis. The procedure allows for both diagnostic assessment and therapeutic interventions.
What are the advantages of knee arthroscopy?
Knee arthroscopy offers several advantages, including smaller incisions, reduced scarring, faster recovery times, and less postoperative pain compared to open knee surgery. The minimally invasive approach allows for targeted treatment of specific issues within the knee joint.
What is hip replacement surgery?
Hip replacement surgery, also known as hip arthroplasty, is a surgical procedure in which a damaged or diseased hip joint is replaced with an artificial joint, called a prosthesis, to relieve pain and improve mobility.
What are the types of hip replacement surgery?
There are several types of hip replacement surgery, including total hip replacement (replacing both the ball and socket of the hip joint), partial hip replacement (replacing only the ball portion of the hip joint), and hip resurfacing (reshaping the damaged bone and capping it with a metal prosthesis)
What are the potential risks and complications of hip replacement surgery?
Potential risks and complications of hip replacement surgery include infection, blood clots, dislocation, implant loosening or failure, nerve or blood vessel injury, and complications related to anesthesia. Patients should discuss these risks with their surgeon before undergoing surgery.
What activities can I do after hip replacement surgery?
Following hip replacement surgery, most patients can engage in low-impact activities such as walking, swimming, cycling, and golfing. However, high-impact activities or sports that involve running, jumping, or heavy lifting may need to be avoided to prevent implant wear or damage.
When can I return to work after hip replacement surgery?
The timing of returning to work depends on factors such as the type of work performed, the physical demands of the job, and the individual's rate of recovery. Most patients can return to light-duty or sedentary work within a few weeks to months after surgery, while those with physically demanding jobs may require a longer recovery period.
What are the risks of ceramic hip replacement?
Like other surgeries, ceramic hip surgery has some risks including:
- Reaction to anesthesia
- Infections
- Excessive bleeding
- Blood clots.
What are the symptoms of a multiligamentous knee injury?
Symptoms may include
- severe pain
- swelling
- instability or a feeling of the knee "giving way,"
- inability to bear weight on the affected leg, and limited range of motion.
What are the treatment options for a multiligamentous knee injury?
Treatment depends on the severity of the injury and which ligaments are involved. It may include conservative measures such as rest, ice, physical therapy, and bracing, or surgical intervention to repair or reconstruct the damaged ligaments.
Can I return to sports or physical activities after a multiligamentous knee injury?
With proper treatment and rehabilitation, many patients can return to their previous level of activity. However, it's crucial to follow the guidance of your healthcare provider and sports medicine team to ensure a safe return to sports or physical activities.
What is a growth factor injection for OA knee?
A growth factor injection involves the use of concentrated growth factors, typically derived from the patient's own blood (autologous), to promote healing and tissue regeneration in the knee affected by osteoarthritis.
What types of growth factors are commonly used in these injections?
Commonly used growth factors include
platelet-derived growth factor (PDGF)
transforming growth factor-beta (TGF-β)
insulin-like growth factor (IGF), and vascular endothelial growth factor (VEGF).
How is a growth factor injection administered?
The procedure involves
- Drawing a small amount of blood from the patient
- Processing it to concentrate the growth factors
- Then injecting the concentrated solution directly into the affected knee joint under sterile conditions, often guided by imaging techniques such as ultrasound.
How soon can patients expect to experience improvement after a growth factor injection?
The timeframe for experiencing improvement varies among individuals. Some patients may notice relief within a few days to weeks after the injection, while others may require more time to see significant benefits.
The duration of pain relief and improvement in symptoms can vary. Some patients may experience longlasting benefits for several months to years, while others may require periodic injections to maintain results.
Patient Stories
Our patients are our best advocates, hear the inspiring stories of their treatment journey
Blogs
The source of trustworthy health and medical information. Through this section, we provide research-based health information, and all that is happening in Aster Hospital.