Mechanical heart valves are recommended in mitral valve disease patients aged <65 years with a reasonable life expectancy and no contraindications to long-term anticoagulation. This recommendation was made because of the durability of the mechanical prosthesis over bioprosthesis. However, the durability of the mechanical valve is often challenged by obstructive thrombus as early as the first year. The mechanical heart valve thrombosis incidence ranges from 0.1% to 5.7%. Redo surgery or fibrinolysis in high-risk surgery patients is the currently available evidence-based treatment. Redo cardiac surgery often ends in a new valve replacement with a bioprosthetic valve though isolated reports of thrombus or pannus removal are available in the literature. Ultraslow infusion of fibrinolysis has shown promise over bolus fibrinolysis. Failure to release the stuck leaflets, embolic stroke, and systemic embolism are known complications of systemic thrombolysis. However some for patients thrombolysis or urgent re-do surgery is not feasible due to various patient speciific conditions. The current case represents this subset of the population, where surgery or fibrinolysis was not the most appropriate option to imorove chances of survival.
A 40 year male patient, known case of rheumatic heart disease withe severe MR and AS had undergone Mitral plus aortic valve replacement 3 years ago with st jude mechanical valves (figure 1). Mechanical valves need lifelong anticoagulation with Vitamin K Antagonists (VKAs) to prevent smooth finctioning without developing thrombosis. One of the most important point to note is VKAs (like Warfarine or acenocoumarol) have very low therapuetic window (that is their therapeitic levels fluctuate a lot in a given patient and are affected by numerous dietary factors and drug-drug interactions) and hence even for most closely observed patients Time in therapeutic window remains as low as 60%. This patient had missed Warfarin doses in his travelling for 3-4 days.
He presented with syncope, hemodynamic collapse and acute dyspnea to outside hospital, where INR was found to be 1.76. Since he had hemoptysis, he recived Vitamin K and Fresh Frozen Plasma to control bleeding. But hemoptysis was actually due to pulmonary edema (pink frothy sputum of frank pulmonary edema). He worsened rapidly and was gasping hence was electively intibated and put on mechanical ventilation and was referred to aster aadhar hospital for further management.
On arrival patient had pink froth inside endo-tracheal tube characteristic of pulmonary edema, GCS was E1M3VT (5/15), Pulse was 150 beats per minute, Blood pressure was 100/60 mm of Hg on high dose nor-adrenaline infusion, Respiratory system examination had bilateral extensive crepitations with respiratory rate of 50 per minute and gasping respiration and saturation was 88% on volume assist control mode of mechanical ventilation with FiO2 of 100%, PEEP of 8 under sedation and paralysis (Figure 2 - showing patient in critical condition before and after the recovery). Foleyes catheterization was done which yeilded muddy sedient proably indicative of acute tubular necrosis due to prolonged cardiogenic shock (Figure 3 - showing muddy urine on catheterization and improvement in urine appearance after recovery with treatment post PETROS). ECG showed sinus tachycardia and no significant ST-T changes. Emergency HRCT chest was done while shifting from Ambulence to ICU, which showed bilaterals extensive consolidations with components of pulmonary edema and minimal bilateral plural effusion (figure 4 - HRCT images pre procedure and post procedure showing significant resolution of pulmonary edema within 36 hours). Emergency bedside Echocardiography was done which showed normally functioning mitral valve prosthesis withe increased gradients & Stuck aortic valve mechanical prosthesis with gradients of 156/107 mm of Hg, LV function was preserved. ABG showed high lactates and severe metabolic acidosis.
On mechanical ventilation Pulse 145 bpm
BP 126/76 on high dose noradrenaline Saturation 91% on FiO2 100%, PEEP-5
4 days
Hemodynamically stable, off all supports
At this point of time, patient was critically sick and was clinically deemed to have had poor prognosis and slim chances of survival. Thorough explaination regarding patient condition, option of systemic thrombolysis with streptokinase versus Primary percutaneous Trans-catheter release Of Stuck leaflets of aortic mechanical prosthesis was done with patients relatives. Risk of stroke, bleeding, and likely death (due to delayed effect) with Systemic thrombolysis was explained to relatives in the language theu understand the best. Also Cerebral embolic protection devices were not available at that point of time, hence risk of stroke during Primary PETROS was explained. Considering time dependent emergency, patients relatives opted for Primary PETROS with risk of cardio-embolic stroke.
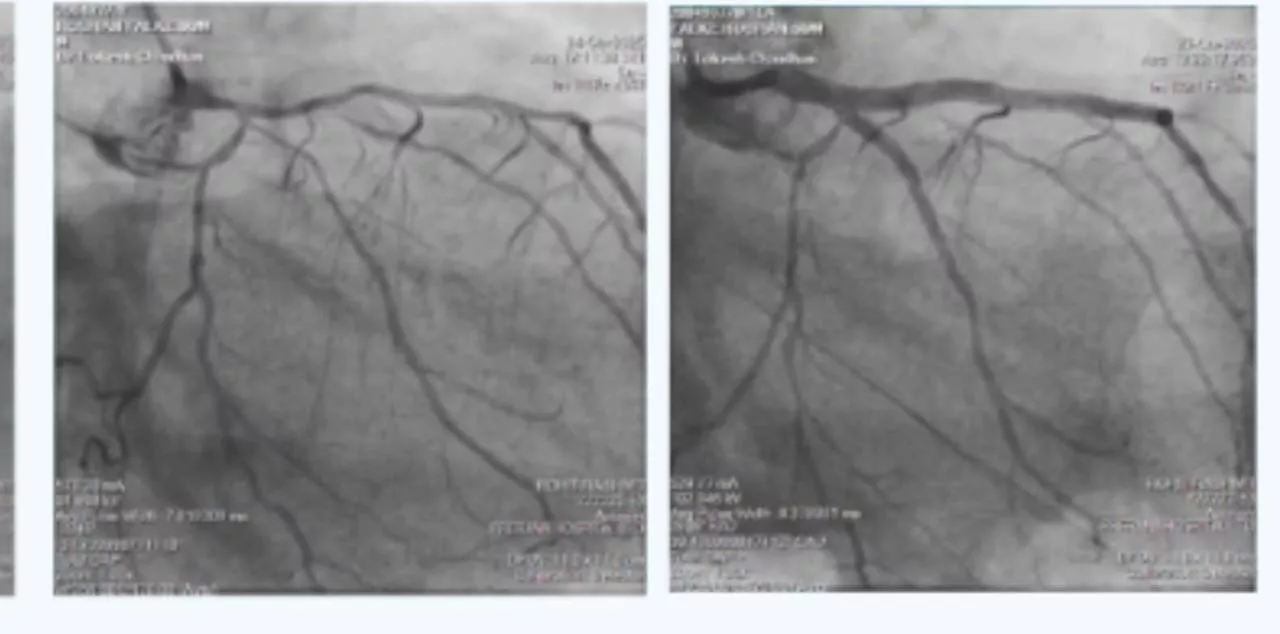
Hence patient was taken up to cathlab for PRIMARY PETROS procedure. First fluroacopy to see leaflet movement of both aortic and mitral mechanical prosthesis was done, which showed stuck aortic mechanical prosthesis with minimal movement of both of its leaflets while mitral valve leaflets were normal. 6F right femoral aterial access was taken. It 6F AL1 catheter with terumo guidewire was advanced till root of aorta.central orifice was crossed using Terumo guidewire into LV and AL1 catheter was advacned over the wire right uptil central orifice of aortic mechanical valve prosthesis.
Then 0.014' Miracle 6 wire was crossed into LV from AL1 cathter. Then central orifice of aortic proathetic valve was serially dilated using 3.0 mm, 3.5 mm and then 4 mm balloons to free the movement of aortic leaflets. Lateral leaflet movement normalised but ledial leaflet movement was still restricted. Hence 0.014' guidewire was recrossed through medial major orifice of the aortic mechanical prosthesis and was balloon dilated using 4.5 and 5 mm balloons serially, which lead to normalization of medial leaflet movement (Figure 5 - fluroscopy images before, during and after the PETROS procesure). Echo done immidietly post procedure showed fall in gradients from 107 mm Hg mean to 30 mm Hg. After successfull procedure patient was shifted back to ICU and heparin infusion titrated with 6 hourly ACT was started. Patients FiO2 and PEEP requirements gradually reduced and became minimal, inotropic requirement also came down significantly within 24 hours, chest Xray improved signficantly and HRCT showed significant improvement at 36 hours (figure 4 showing HRCT images before and after the procedure). After 48 hours patient was extubated and put on O2 via face mask. But remained drowsy for next 48 hours. Hence neuro imaging was done which did not reveal any abnormality, hence flumazenil challenge was done which showed signficant improvement in sensorium. Hence watchfull waitig for GCS was continued and eventually he regained complete sensorium with spontaneous movements of all 4 limbs. Got mobilized out of bed on Day 5 of admission. And was started on oral VKA again overlapped with LMWG till INR was more than 3. Subsequently when INR was more than 3 on day 9 was dischaged in stable condition.