Introduction :
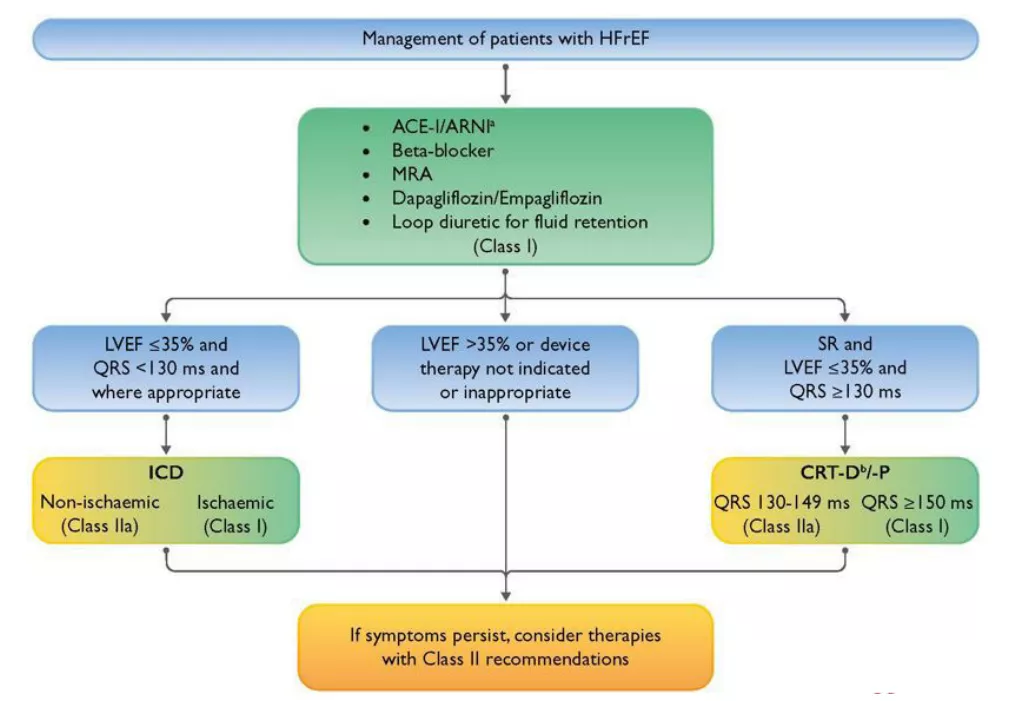
Heart failure with reduced ejection fraction (HFrEF) is complex disease which requires a specialized care. Treatment involves treating underlaying conditions such as valvular or ischemic heart disease along with guideline directed medical therapy (GDMT) Fig 1. Four important classes of drugs in GDMT are ACE inhibitors ( or newer ARNI ), beta blockers, SGLT2 inhibitors and mineralocorticoid inhibitors (MRA). However some patients who remain symptomatic on GDMT can be offered device based therapies like CRT -P/D which is based on electrical synchronization of heart which results in better ejection performance of the failing heart. Current indication of CRT includes patients of refractory heart failure with severe LV systolic dysfunction who remain symptomatic on GDMT with QRS duration more than 150 ms. Addition of defibrillation therapy depends on scar burden and likelihood developing ventricular arrhythmias. Although CRT implantation it is safe procedure, but complications can sometimes happen which require prompt action. Presenting here a case of CRT-D implantation which got complicated by cardiac tamponade due to lead perforation which was managed successfully by combined cardiac -CVTS team effort.
Case history :
A 70 years female with history of PTCA + stent to LAD to diagonal done three years back at another centre was evaluated at our hospital for worsening dyspnea. Her ECG showed Complete LBBB with QRS duration of 160 ms (Fig 2). She was currently symptomatic with NYHA class IV dyspnea while on optimal dose of GDMT and moderate to high dose of diuretics. Her echocardiographic study showed EF of 25% with recent decline to 20%. Check angiography showed patent stent in LAD to Diagonal. Cardiac MRI showed reduced EF of 20% with large scar on anterolateral wall (scar burden more than 25% of myocardium). Based on this data decision to implant CRT-D was taken and patient was admitted for the same.
CRT-D implantation :
Patent underwent successful CRT -D implantation via left subclavian approach with RA lead, RV mid septal lead (AICD lead) & LV lead via coronary sinus under angiographic guidance (Fig 3.) Electrical parameters of all three leads were excellent with very significant reduction in QRS width, hence pulse generator was implanted and wound was closed. 12 lead ECG post CRT was show narrow QRS with QRS duration less than 110 ms (Fig 4). Patient was given pain management and antibiotics and remained hemodynamically stable on day of surgery. Next day after seeing Echo, ECG and CXR patient was shifted to room there was no pericardial effusion noted on bedside echo, x ray showed lead position was intact and ECG showed good narrowing of QRS with paced rhythm.
Post procedure course :
After patient was shifted to room, she remained stable for entire day except few bouts of coughing. In later evening patient developed sudden hypotension so she was shifted back to ICU. Her blood pressure was 80/60 and heart rate 70 per minute, In ICU we did repeat ECG which showed paced rhythm with no fresh changes compared to post procedure ECGs. Bedside CXR showed normal lead positions. Echo showed large echogenic collection in posterior and lateral part of LV causing cardiac tamponade, this was suggestive of clotted blood in pericardium. Emergency pericardiocentesis was attempted and 7F sheath was inserted in pericardium under echo guidance. However there was no free flow while aspiration as clots are would not come out through sheath. Nevertheless tapping still helped in this situation as whatever small amount of serous fluid aspirated helped to temporarily relieve/reduce tamponade effect while CVTS team was on its way. Condition was explained to relatives and patient taken to OT for sternotomy and open surgical drainage of clots in pericardium.
Surgeon’s perspective and intra-operative management :
As the patients condition deteriorated, after temporary improvement due to pericardiocentesis, we decided to explore her through a sub xiphoid incision.
Inside the theatre, we entered the pericardial cavity through sub xiphoid incision, but seeing the amount of clots, it was decided to do a formal sternotomy to have a better control of the situation.
On pericardiotomy through sternotomy, we encountered huge clots all over, which were removed. On examination we found a small tip of the pacing wire protruding out through RV free wall just adjacent to the mid LAD. No active bleeding seen at that time. As it was just the tip of the pacing wire and the patient could not have been transferred to the Cathlab, it was decided to just fix it in the OT itself. We stitched a small patch of pericardium over the tip to cover the pacing wire, preventing its further advancement and to keep it away from the adjacent LAD. As there was no active bleeding now, we closed the chest as routine protocol.
Post operative management :
Post sternotomy and surgical drain + patch, patient made rapid hemodynamic recovery and was extubated next day. She required 2 packed cells transfusions. Renal function and urine output remained normal. Pericardial drains removed on day 5 after serial echo studies showing no re-collection of blood in pericardium. Her ECG and Lead parameters were monitored closely and remained within acceptable limits. Patient was discharged after 1week of surgical intervention in stable condition.
Follow up :
Patient completed 2 moths follow up. She is asymptomatic now with no dyspnea at present. Serial ECGs show narrow QRS (110 ms), EF improved to now about 35%. She is now doing very well on ARNI, SGLT2 inhibitors, and MRA and loop diuretics have been stopped now.
Discussion :
Cardiac tamponade is a rare complication following CRT implantation. Most common cause is lead perforation. Technically any lead can perforate but most of the times it is the ICD or LV lead. Fresh bleeding in pericardium can be managed usually by pericardiocentesis. Perforated lead often needs careful repositioning if there is ‘loss of capture’ by the lead or if its electrical parameters (threshold, impedances) are significantly deranged. Our case here had some unique features. Firstly, only the tiny portion lead tip had perforated through to the surface and majority of pacing portion of lead was still inside myocardium- due to this its pacing function was still intact suggested by normal RV lead capture on ECG and normal lead parameters on pacemaker interrogation. As the perforation was partial (or contained) it resulted in single self-limiting bout of bleeding which later on clotted requiring evacuation. Only concern was continued forward migration of lead may have needed its repositioning requiring series of re-interventions. But this was taken care by innovative and mindful surgical patching of lead tip preventing its progressive movement. After this co-ordinated cardiology -surgical management we were able to prevent almost inevitable lead repositioning, which would have required a 3rd procedure in a frail elderly person. Over last 2 moths of follow up her ECG shows paced rhythm with narrow QRS and lead parameters assessed on serial device interrogation have remained stable. This entire management has also translated into improvement in LVEF, clinical improvement and better quality of life.