Constipation
When am I constipated?
It is a common misunderstanding that not passing motion is constipation. However, constipation truly means that there is a change in your normal bowel habits, to cause discomfort in your tummy.
What are the signs to look for?
If you are going through any change in bowels habits as listed below, you should inform your doctor.
- Firm/ Hard stools
- Straining to pass stools/ taking longer in the bathroom than before.
- Pain while passing stools
- Feeling of incomplete emptying
- Bloated feeling in tummy
- Tummy cramping pains
- Nausea along with abdominal discomfort.
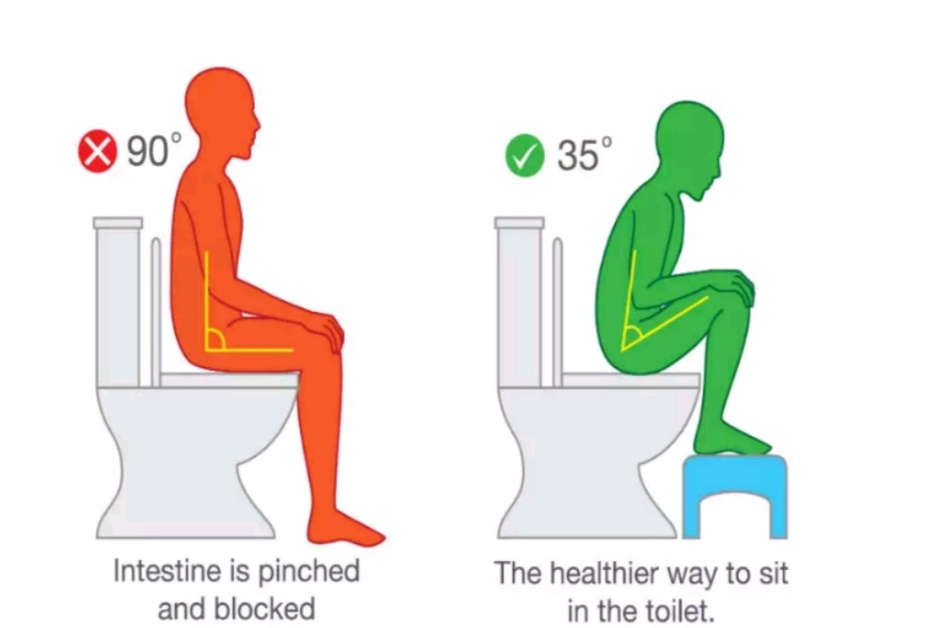
Right Position for passing motion
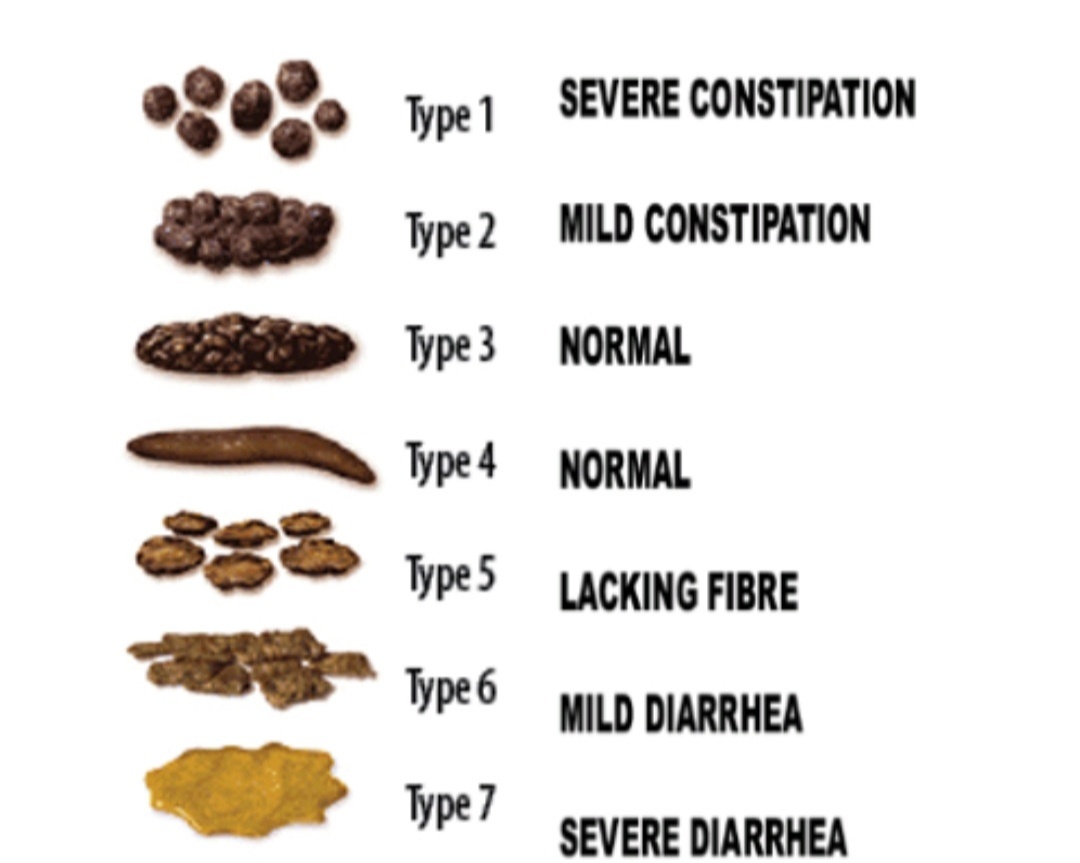
Easy scale to guide level of constipation: Bristol stool scale
What can I do?
- Eat Enough Fiber
- Drink plenty of water – about 2 liters a day
- Exercise everyday
- Do not resist the urge to go to the bathroom
- Position yourself as shown in the picture
- Discuss with a nutritionist about foods rich in fiber
- Inform your doctor if there are concerns
- Follow the instructions prescribed without fail
What are the possible complications?
- Overflow diarrhea
- Abdominal pain
- Urinary retention
- Hemorrhoids/ Piles
- Cuts (fissure in ano)
- Confusion/ Delirium
- Intestinal obstruction
Lymphedema
What is lymphedema?
In order to understand what lymphedema is, we will first have to understand what the lymphatis system is.
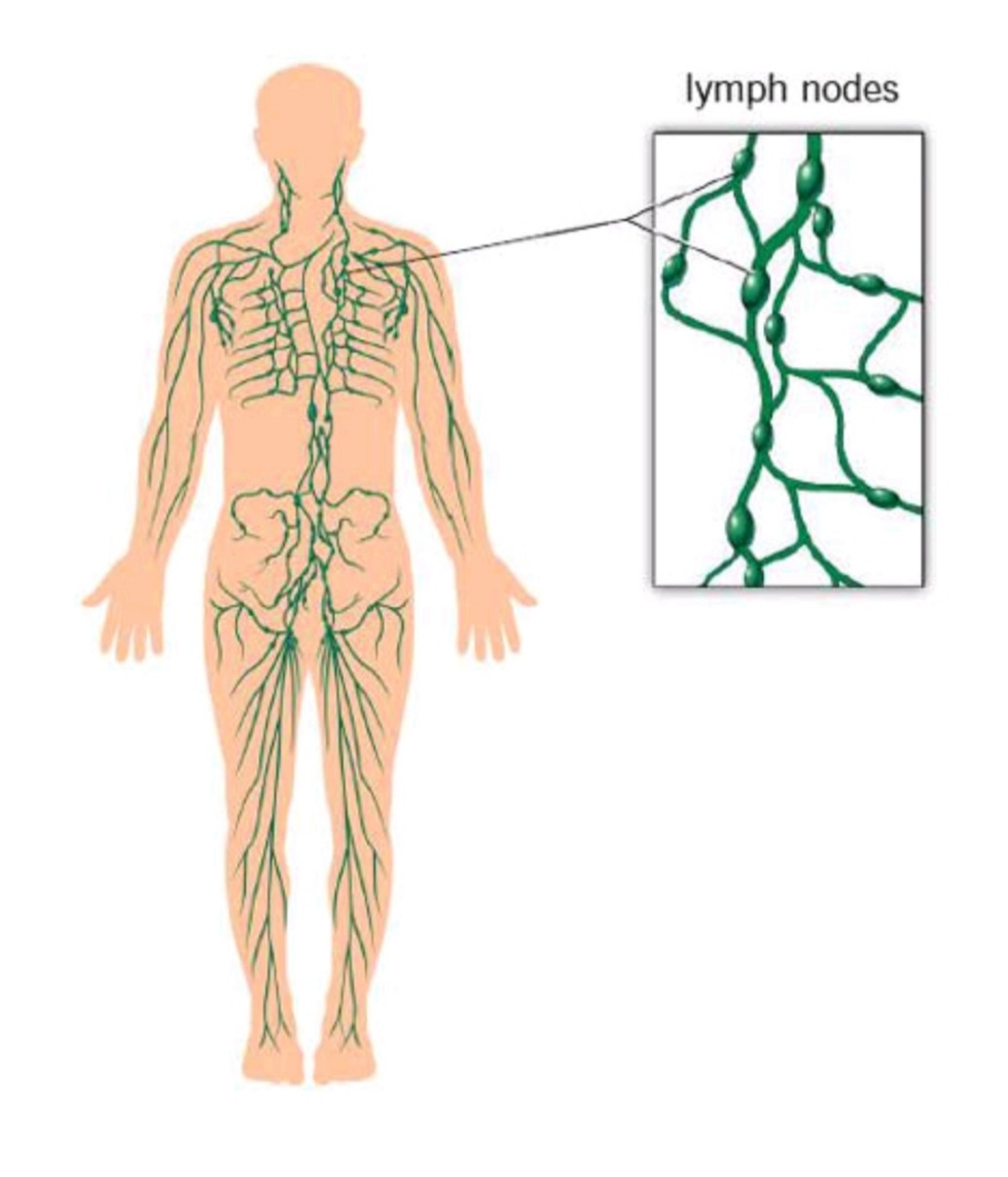
Lymphatic system
When you see your arms, you see the bulging vessels that collapse under pressure. These are veins that take majority of the blood from the body back to the heart. There is however, some fluid inbetween the tissues and under the skin that needs draining. This is drained by a group of specialised vessels called lymphatics that finally join the big veins in the body. The fluid that they drain is called lymph. These vessels go through groups of nodes that are situated at various levels in the body. These nodes are called lymph nodes
Lymphedema:
After surgery or radiation therapy for malignant lumps, these nodes are also taken out and some of the lymph vessels are also taken out. This essentially means that the draining of the fluids in the midst of tissues is decreased, causing the part of the body it drains to swell up. This is called lymphedema.
What are the features to watch for?
- Gradual feeling of heaviness in the limb on the side of procedure
- Clothes feeling a bit tighter
- Skin may feel tight/ stretched/ itchy
- This progresses to swelling that is seen through the day but decreases on resting
- Swelling will Increase gradually if not attended to, skin will become firm and rough, swelling will not decrease.
- Neck pain due to the heaviness in the limb/ after surgery
How to care for the limb that has lymphedema?
There are 4 cornerstones of managing the limb
- Skin Care
- Clothing should be loose and made of pure cotton.
- Ensure skin is kept moisturised – coconut oil is excellent. If - using other creams – use non-fragranced ones as they will not cause skin irritation.
- Do not scratch the skin. The fluid is food for bacteria and will get infected.
- Do not allow BP monitoring/ blood collection/ IV cannulation in that arm
- Ensure that every few hours you rest for 45minutes and keep the arm elevated. - Exercise:
It is important to do the exercises taught by the lymphedema Nurse Specialist. The lymph vessels run through muscles, that act as a pump to help improve the return of collected fluid. - Massaging:
The flow of collected fluid can be directed through these massages, that are done in a particular way, towards the functioning lymphatic vessels. This is called Manual Lymphatic Drainage Therapy. - Compression bandaging:
- Compression garments. It is better to use ones that are tailor made for you specifically. This will prevent pain and trauma of the skin. These garments can be used in the initial stages of lymphedema, but as the lymphedema worsens, these will not be sufficient
- Lymphopress – Pneumatic compression technology – improves lymphatic flow
- Multi-layered compression dressing which will be taught to you by your lymphedema Nurse Specialist. To have optimal effect, they have to be worn for about 10-12 hours continuously and simultaneous exercises to be done.
Important facts:
Having lymphedema is not easy. There are challenges faced, that affect you emotionally, psychologically and financially. It is important to:
- Voice your concerns to your doctor/ Lymphedema specialist Nurse
- Have open communication with your family
- Family support is essential
- It is equally important for the family to express their concerns as they care for you
- Empowering the family to help you is most important part of care
Team there to help you:
- Primary physician – actively manages your care
- Pain Specialist – helps with pain of any cause
- Lymphedema Specialist Nurse – who will guide management
- Rehabilitation Specialist – helps you get back maximum function
- Physiotherapist – ensures the exercises maximise effect of treatment
- Psychologist – who will empower family and you in ways to cope
- Occupational therapist – Who will help you cope with your daily activities
- Mind and Body Medicine – will help you find ways to relax mind and body.
What are the situations to seek help:
- When there is sudden increase in the limb
- If there is increased redness in the limb
- If there is fluid leaking from the limb
- Fever and rashes on the limb
- Increased pain from any cause
- If there is increased distress of any cause – physical, emotional, psychological
- Sleep disturbance
If there are any concerns please contact Multispecialty Clinic - Pain, Palliative and Rehabilitation Department. Aster CMI Hospital, Bengaluru
Mucositis
What is Mucositis?
Our digestive system – that is, from mouth to the rectum, is lined by a soft, wet slimy substance called mucous, that keeps it safe and moist. When this barrier is affected due to medications/illness/chemotherapy/radiation, it can cause inflammation and ulcers to form on this lining. This is called mucositis.
What does it cause in the mouth?
- Pain in the mouth
- Difficulty in swallowing
- Bleeding in the mouth
- Ulcers in the mouth
- Bad smell in the mouth
- Pus in mouth
- Decreased sleep
- Anxiety
- Depression
- Decreased appetite – dehydration, loss of weight, nutritional deficiency, gaps in the treatment plan
What can it cause in the tummy?
- Abdominal discomfort
- Abdominal pain – crampy
- Decreased appetite
- Increased frequency of stools
- Watery stools
- Irritation at the rectal area
Overall it will affect you with:
- Increased stay in hospital
- Increased expenditure on treatment
- Nutritional deficiency
- Gaps in treatment plan
- Reduction in quality of life
What can increase the chance of mucositis or make the mucositis worse?
- If oral health was poor before starting treatment/ while treatment ongoing
- Habits such as eating paan, smoking, alcohol consumption
- If nutritional status and hydration are poor before treatment
- If there are other chronic conditions such as diabetes
- The history of medications needs to be shown to your doctor
- Mouth breathing
- Ill-fitting dentures
- Concurrent chemotherapy and radiation
- Dry mouth
- Depends on the chemotherapy regimen
- Depends on the location of the malignancy
What can be done?
Although it may not be possible to eliminate mucositis with the treatment, it is important to know that reducing the severity is in your hands.
| Oral care | Food | When to be alert doctor |
|---|---|---|
| Maintain good oral hygiene | Avoid spicy foods | If there are ulcers |
| 100ml of lukewarm water + pinch of salt + pinch of baking soda is mixed and used to gargle before and after meals | Avoid eating hot foods (temperature) | If there is difficulty swallowing, abdominal pain, abdominal discomfort |
| Keep your lips moist with water-based lip gels | Keep mouth moist with frequent sips of water | If there is bleeding in mouth, if there is increased diarrhoea |
| Change old habits such as smoking | Eat frequently, small amounts | If oral intake has decreased If urine output is decreasing |
| If you are having radiation, please use the gargles given by your radiation oncologist The protocols are tedious, but it is important to follow them | ||
If there are any queries, please contact: Multispecialty clinic - Pain, Palliative and Rehabilitation Department Aster CMI hospital, Bengaluru
Ostomy care
What does an Ostomy mean?
An Ostomy means, an opening done surgically, through your abdominal wall, that communicates with a hollow organ within your body.
Why an ostomy?
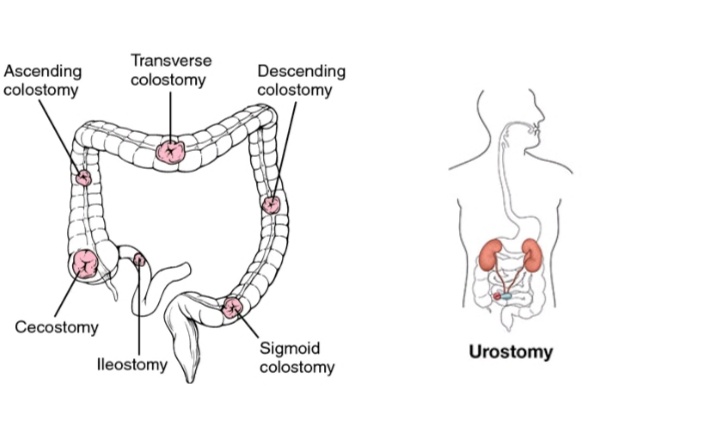
This procedure will be suggested as there is a block in a hollow organ in the body such as intestine/urinary tube. There are 2 types:
- One that allows waste material from the body to come out – output ostomy – colostomy, Ileostomy, Urostomy, Venting gastrostomy.
- One that allows nutrition to be given to the body – Input Ostomy - Percutaneous endoscopic gastrostomy (PEG), Jejunostomy.
The ostomy can be for a while (temporary) or permanent.
What should I know about Ostomy care?
What is a pouch?
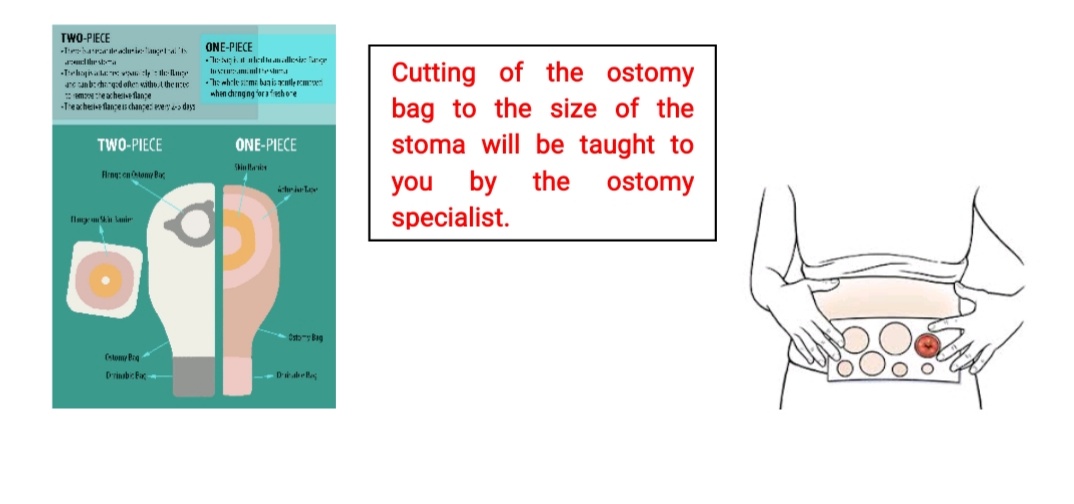
When you have an ostomy, it is protected with a pouch, which also is used to collect the waste products from the body such as stools, urine. There are 2 types of pouch:
- One which can be used only once and discarded.
- One which has 2 parts - one called the wafer - stuck to the skin on the tummy, and the pouch - which is connected to the wafer. The contents can be emptied every time it fills.
Where are the Stoma's located?
How do I look after the pouch?
Changing The Pouch:
For the first 48 hours, the pouch you will have will be transparent, as the stoma will change to adjust to its function. Following this, the pouch will be one which is non-transparent. The choice of single use or multiple use pouch is yours. The way to change the pouch will be taught to you, by staff specialised in the management of pouches and stoma.
Emptying The Pouch:
There is always a concern that there will be embarrassing leakages from the pouch. The important thing to remember is that while this cannot be avoided on an odd occasion, this is easily managed.
Important Facts To Remember:
- Ileostomy and ascending colostomy – bowel movement is watery and can fill the bag more frequently
- All other colostomy – formed stools. Usually once to twice a day filling noted.
What To Do:
- Empty the pouch when 3/4th full with bowel movement
- If filled with gas (flatus), empty the bag
- Always carry a send bag with you if travelling or going out.
Other concerns when having an ostomy:
- There is no concern while having bath.
- There are certain foods that can increase the flatus production. You will have to keep a record of what foods you are sensitive to. You will be able to eat almost all foods.
- Odour from the pouch - pouches now come with filters of activated charcoal in them, and this takes care of the odour.
- Drink plenty of water.
- While travelling by public transport, ensure the ostomy bag is protected
- Always take extra clothing with you.
- Do not wear tight clothing
- Return to sexual activity is a positive experience if your outlook of body image is positive. There are suggestions on how to make it a positive experience, that our team can help with.
- Avoid lifting heavy weights, doing robust exercises or aggressive games or contact sports.
- Apart for the first few months after the surgery, you can resume most of your daily chores and activities.
- Always discuss concerns with your doctor/ ostomy team.
Please contact your doctor or ostomy nurse immediately if you experience any of these:
- Abdominal pain/ distention/ persistent vomiting
- Constipation/ diarrhoea
- Any skin irritation at the site of wafer/ leakage
- Any change in appearance of the stoma
If there are any concerns please contact: Multispecialty Clinic – Pain, Palliative and Rehabilitation Department Aster CMI Hospital, Benagluru
Understanding common oral condition
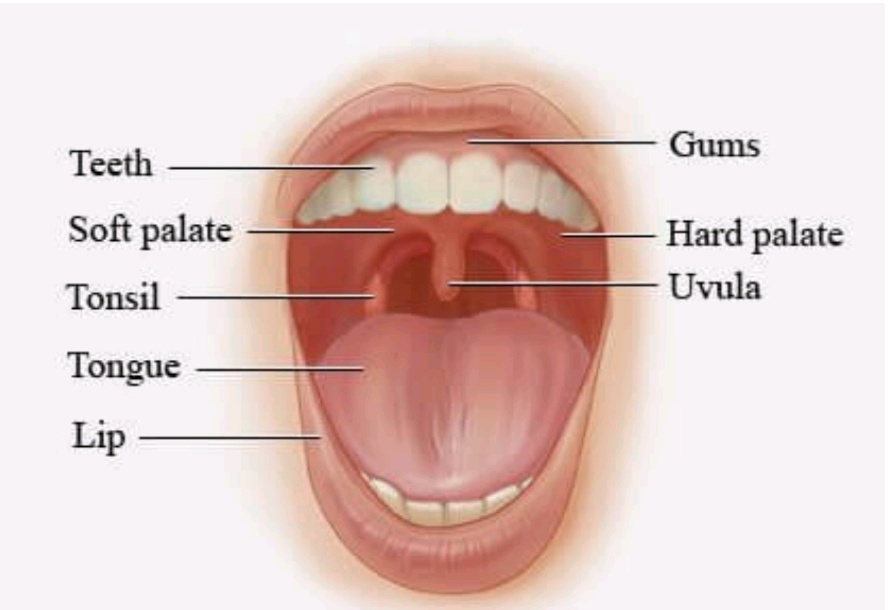
Parts of the mouth:
Oral care is important as it affects the quality of life of a person.
| Healthy Oral cavity | |
|---|---|
| Lips | Moist, no cracks/ ulcers in angle of mouth |
| Gums | Pink, no plaque/ bleeding |
| Tongue | Pink, no coating/ white patches/ ulcers |
| Palate | Pink, no ulcers/white patches/bleeding |
| Mouth | Saliva present, bad breath smell |
| Throat | No redness/pus/bleeding/ulcers |
| Teeth | No chipped teeth/decay/cavities |
What are the problems affect the mouth?
Mouth is a very important part of our body. It is where we taste our food, feel thirst and speak. Anything that causes a change in the balance of the saliva in our mouth can cause discomfort and problems that distress. These can affect any individual. Some of them are:
- Dry mouth
- Burning in the mouth and lack of taste
- Bleeding gums and Smell in the mouth
- Ulcers and infections in the mouth
Dry Mouth
Saliva in the mouth keeps our mouth moist and is produced by glands in the mouth called salivary glands. If the production is less, then the mouth can go dry.
Caused By:
Mouth breathing, drinking less water, anxiety, smoking, chewing tobacco, diabetes, conditions that affect the salivary glands.
How Does It Affect You:
Lack of taste, disturbed sleep, difficulty in chewing and swallowing, ulcers in the mouth, difficulty in talking to others, bad smell in the mouth. Sometimes, it can cause a fungal infection called candidiasis.
Burning in mouth and lack of taste
Any part of the mouth can be affected – lips, gums, inner cheeks, palate, throat. The taste buds are on the tongue and our taste depends on the taste buds working well. Sometimes, these are damaged
Caused By:
Dry mouth, fungal infection, nutritional deficiencies, allergies, intense gastritis, with regurgitation to the mouth, poor oral hygiene, diabetes, anxiety.
How Does It Affect You:
You could have difficulty in eating, intense loss of taste in the mouth, bitterness, stinging even to water, difficulty in sleeping at night.
Bleeding Gums and Bad smell in mouth
Caused By:
Poor oral hygiene, plaque causing irritation and swelling of the gums, vitamin deficiencies, some illnesses that cause bleeding.
How Does It Affect You:
Pain in the mouth, burning in the mouth, difficulty in chewing, makes social speaking difficult, bad smell in mouth, infections if not treated. If there is constant, easy bleeding from gums, you should visit your doctor and dentist at the earliest.
Ulcers and infections in the mouth
The saliva and the mucous content in the mouth keep the mouth healthy. Any of the above conditions can cause the protective layers to be destroyed. Our mouth normally has bacteria in it. When this protective layer is destroyed, ulcers can happen and these can worsen due to the bacteria in the mouth.
Caused By:
Vigorous brushing of teeth, cleaning gums with metal cleaners, injury due to dental appliances, dentures, sensitivity to certain foods, vitamin deficiencies, stress, it can be an indication of illness that require immediate attention such as herpes infection, celiac disease, inflammatory bowel disease, diabetes mellitus and issues with the immune system.
How Does It Affect You:
Pain in the mouth, burning in mouth, difficulty in chewing, smelly breath, difficulty in speaking, increased salivation, sleep disturbance, emotional distress.
Care of the mouth:
- Ensure brushing at least twice a day
- Use toothpaste that has a minimum of 1350 parts per million of fluoride. This information is on the labels of toothpaste.
- Drink plenty of water
- Rinse mouth well after meals
- Speak to your dentist regarding foods to be avoided according to your dental health
- If any of the above conditions are present contact your doctor immediately
- Have a regular consultation with your dentist
Care for Dentures:
- Clean dentures daily.
- Remove at night and whenever possible to expose gums to air.
- Loose fitting dentures can irritate the mouth and gums and should not be worn.
- Do not wear dentures if mouth sores are severe.