Case Summary
A 13-year-old girl presented with:
Intermittent high-grade fever for 1 week
Nausea and vomiting for 3 days
Swelling of hands and feet for 2 days
She had a history of exposure to SARS-CoV-2 one month prior, but remained asymptomatic at that time.
On admission, she was:
Febrile
Tachypneic and tachycardic
Hypotensive
Noted to have pulsus paradoxus
Elevated jugular venous pressure
Facial puffiness and peripheral edema
Decreased bilateral basal air entry
Distant heart sounds
Hepatomegaly was present, and the umbilicus was everted, suggesting fluid overload.
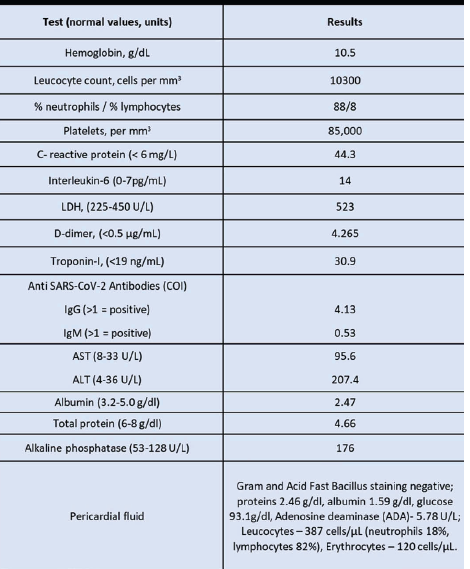
Her RT-PCR for SARS-CoV-2 was negative, but anti–SARS-CoV-2 IgG antibodies were positive, indicating prior exposure. Laboratory investigations revealed markedly elevated inflammatory markers.
Investigations
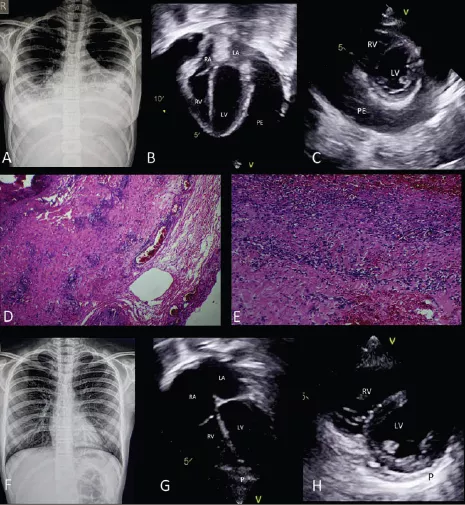
Chest Radiograph
Cardiomegaly (Fig 1)
Bilateral blunted costophrenic angles suggestive of pleural effusion (Fig 1)
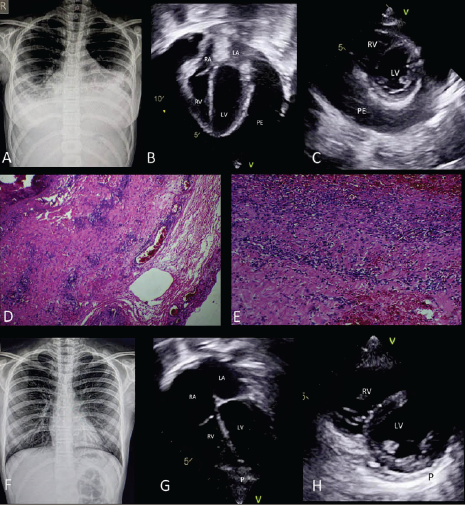
Echocardiography
Structurally normal heart
Massive pericardial effusion
Diastolic collapse of the right atrium and right ventricle
Normal biventricular systolic function
Bilateral pleural effusion
Findings were consistent with the physiology of cardiac tamponade.
Management
Given the presence of massive pericardial effusion with tamponade and bilateral pleural effusions, the patient underwent:
Emergency wide anterior pericardiectomy
Bilateral intercostal tube drainage
Approximately 650 mL of transudative pericardial fluid was drained.
Intraoperative findings:
Intense red discoloration of the epicardium and pericardium
Pericardial biopsy confirmed an acute inflammatory infiltrate
She was treated with:
Intravenous immunoglobulin (IVIG)
High-dose intravenous corticosteroids
Clinical and hemodynamic improvement occurred within 48 hours.
She was discharged after one week (following drain removal) on:
Tapering oral steroids
Aspirin
At 1-month follow-up:
She was asymptomatic
No residual pericardial effusion on echocardiography
Discussion
This case represents a rare and severe presentation of Multisystem Inflammatory Syndrome in Children (MIS-C) associated with prior Coronavirus disease 2019 (COVID-19) exposure.
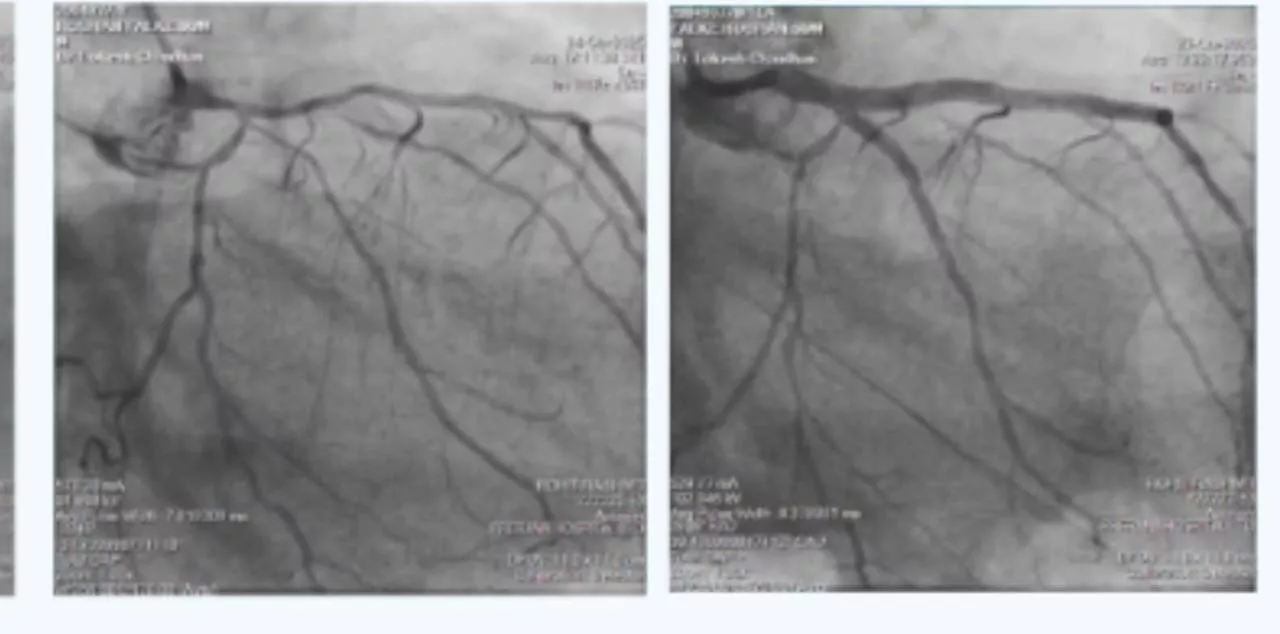
While cardiovascular involvement is common in MIS-C, typical findings include:
Myocardial dysfunction
Coronary artery changes
Mild to moderate pericardial effusion
Severe pericardial effusion progressing to cardiac tamponade is exceedingly rare.
Pericardial involvement in acute COVID-19 is documented, but it is often associated with myocardial injury. In MIS-C, although pericardial effusion may occur, massive effusion requiring urgent surgical intervention has seldom been reported.
This case highlights:
The importance of recognizing pulsus paradoxus and tamponade physiology
The need for urgent echocardiographic evaluation in MIS-C patients presenting with shock
That shock in MIS-C can have multiple etiologies, including rare but life-threatening pericardial tamponade
The potential role of surgical intervention alongside immunomodulatory therapy