Acute Massive Iliofemoral DVT with Pulmonary Embolism in a Middle-Aged Woman after Air Travel
Introduction
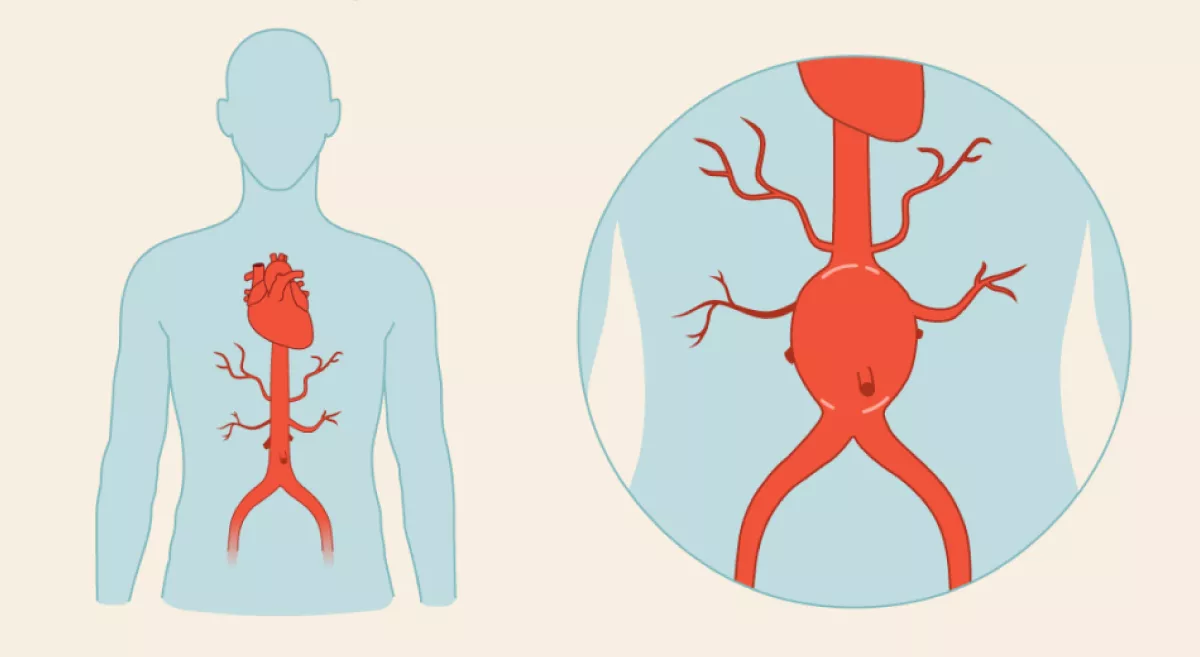
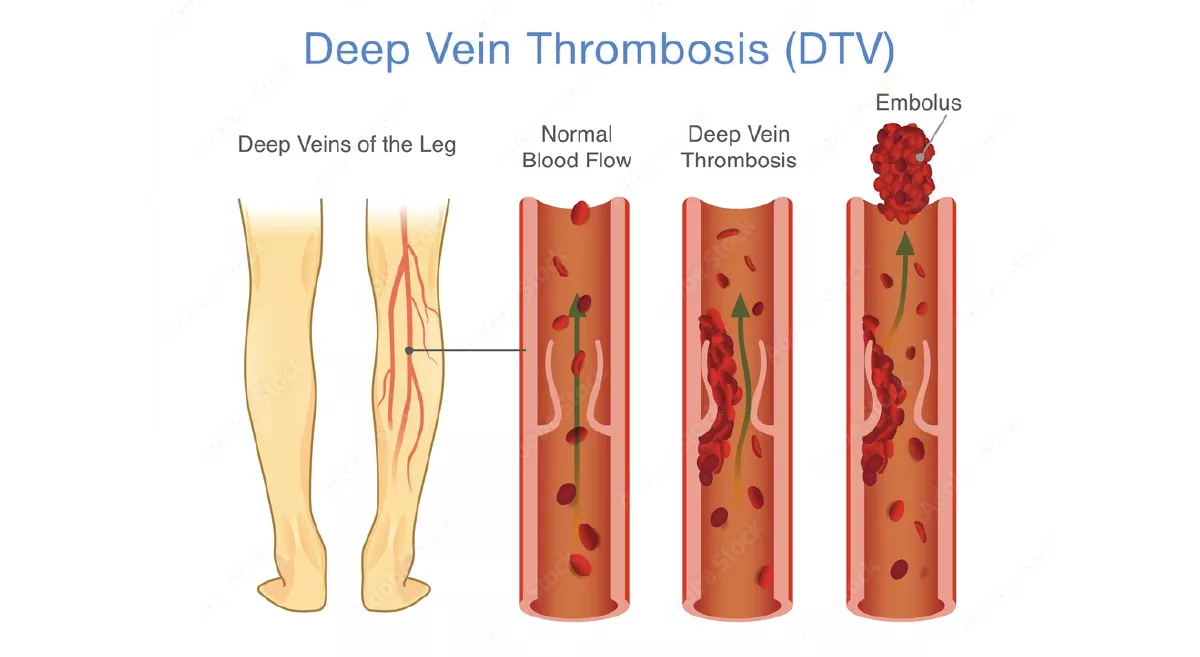
Deep venous thrombosis (DVT) is a life-threatening condition, especially when extensive or associated with pulmonary embolism (PE). Major risk factors include immobility, recent travel, surgery, trauma, and hormonal therapy. Incidence is 1–2/1,000 persons/ year, rising sharply with age. Mortality from untreated PE exceeds 20% in the first month. • Prevalence: 1–2/1,000/year; more common in hospitalised/mobility-impaired. • Morbidity/Mortality: Untreated PE: 20% early mortality. Long-term risk: post-thrombotic syndrome, chronic venous insufficiency.
Case Summary
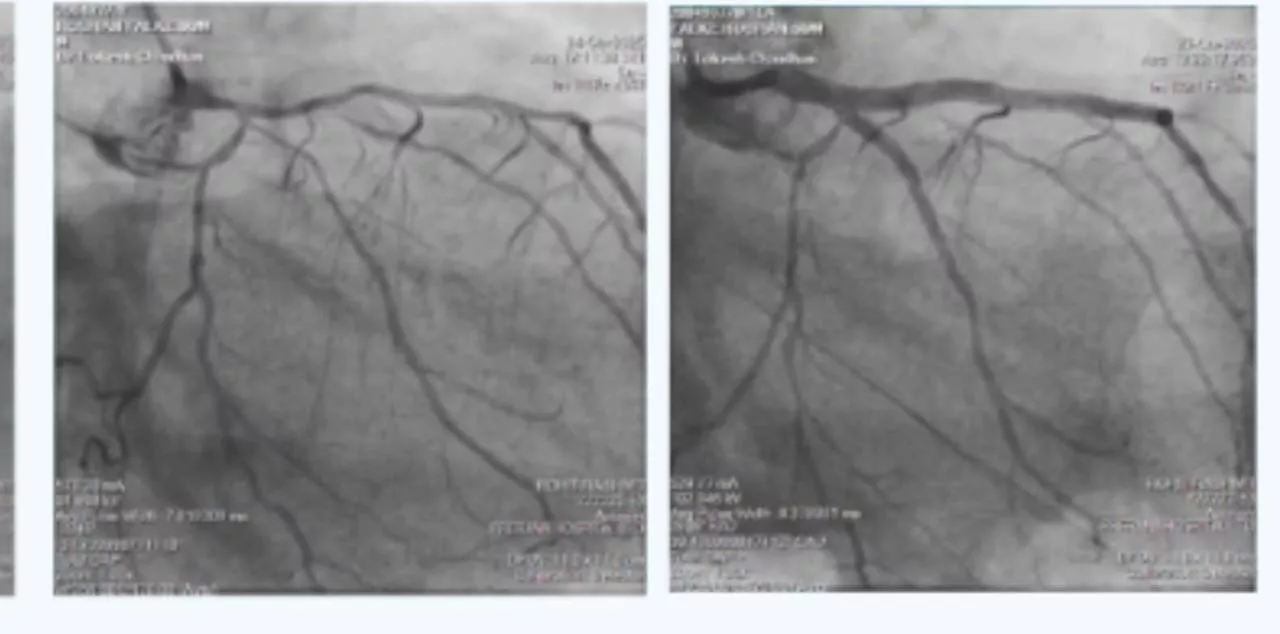
A 48-year-old woman developed a painful, swollen left leg after air travel. Examination revealed diffuse swelling. Doppler confirmed acute iliofemoral DVT and CT venogram showed pulmonary embolism. Management included IVC filter insertion and mechanical thrombectomy using Penumbra device, resulting in complete clearance of thrombus and brisk flow across the iliac veins and IVC.
Discussion Points
- Prompt diagnosis and intervention prevented fatal PE and limb compromise.
- Mechanical thrombectomy is preferred over systemic lysis in massive iliofemoral DVT with high clot burden.
What to look for in your practice
- Suspect DVT in any patient with acute limb swelling and tenderness, especially after immobilisation or travel.
- Early duplex ultrasound is critical – do not delay referral for imaging.
Red Flag Symptoms
- Sudden-onset whole limb swelling
- Discoloration or pain in the calf/thigh
- Breathlessness or chest pain (suggests PE)
When to refer to a vascular surgeon
- Refer immediately for any acute limb swelling and suggestive risk factors.
- Signs of PE (breathlessness, chest pain, collapse) need emergency evaluation.
Follow up in this case
- Therapeutic anticoagulation and antiplatelet therapy.
- Routine imaging surveillance (1 month, 3 month, 6 month and then annually).
- Early mobility and activity. Traditional bed rest is no longer routinely advised.
- Advised to wear graduated compression stockings to minimise the risk of post-thrombotic syndrome (PTS).
- Advised to maintain adequate hydration
Final thoughts
High index of suspicion along with timely clinical diagnosis of DVT in the presence of risk factors, combined with appropriate imaging and prompt intervention, is very important. It prevents life threatening pulmonary embolism in the short term and lifestyle threatening post thrombotic syndrome in the long term.