Follow up in this case
- Therapeutic anticoagulation and antiplatelet therapy.
- Routine imaging surveillance (1 month, 3 month, 6 month and then annually).
- Early mobility and activity. Traditional bed rest is no longer routinely advised.
- Advised to wear graduated compression stockings to minimise the risk of post-thrombotic syndrome (PTS).
- Advised to maintain adequate hydration.
Final thoughts
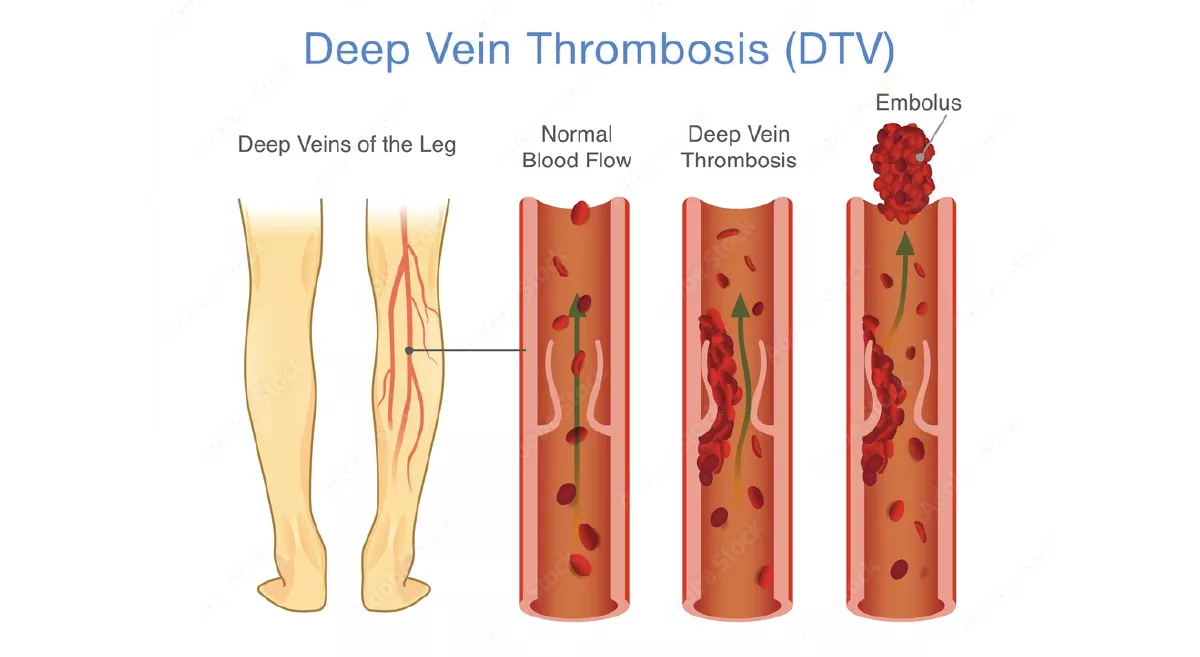
High index of suspicion along with timely clinical diagnosis of DVT in the presence of risk factors, combined with appropriate imaging and prompt intervention, is very important. It prevents life threatening pulmonary embolism in the short term and lifestyle threatening post thrombotic syndrome in the long term.
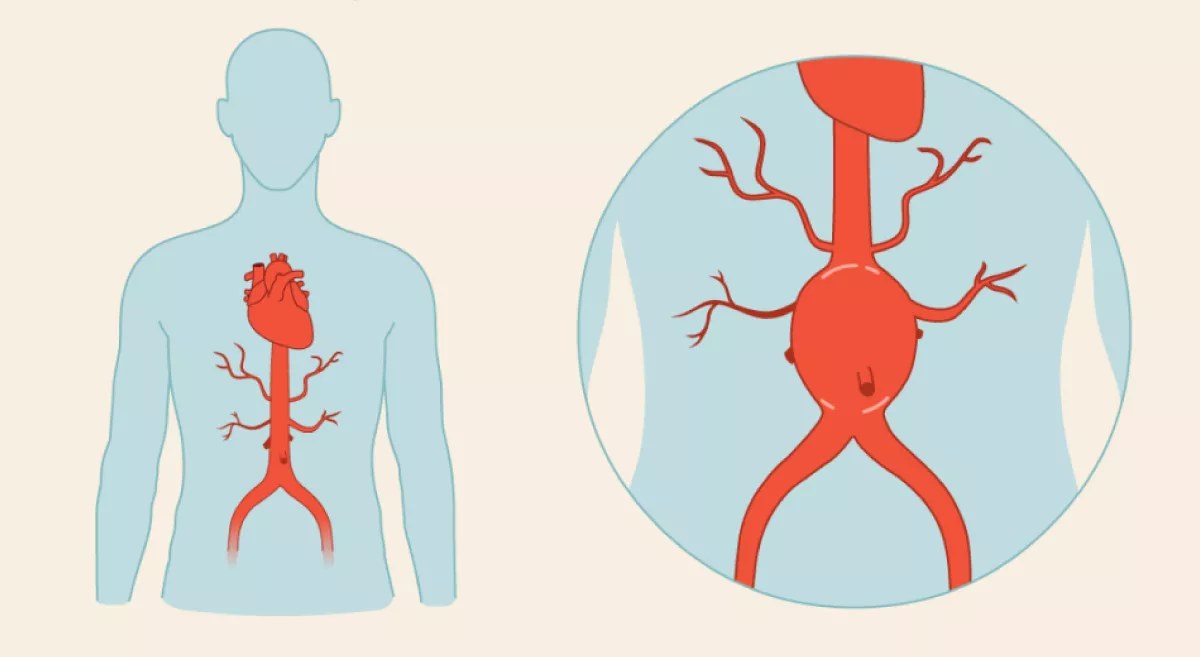
An abdominal aortic aneurysm (AAA) is a ballooning or dilatation of the abdominal aorta, most commonly occurring below the renal arteries. While most AAAs remain asymptomatic, they carry a significant risk of rupture – especially once the diameter crosses 5.5 cm, with a mortality rate of 80–90% if ruptured.
Prevalence:
4–5% in men >65 years
6:1 male-to-female ratio
More common in hypertensives and smokers
Mortality:
Ruptured AAA: >80
Elective open repair: 4–5%
Elective EVAR (Endovascular Repair): 1–2%
Case Summary
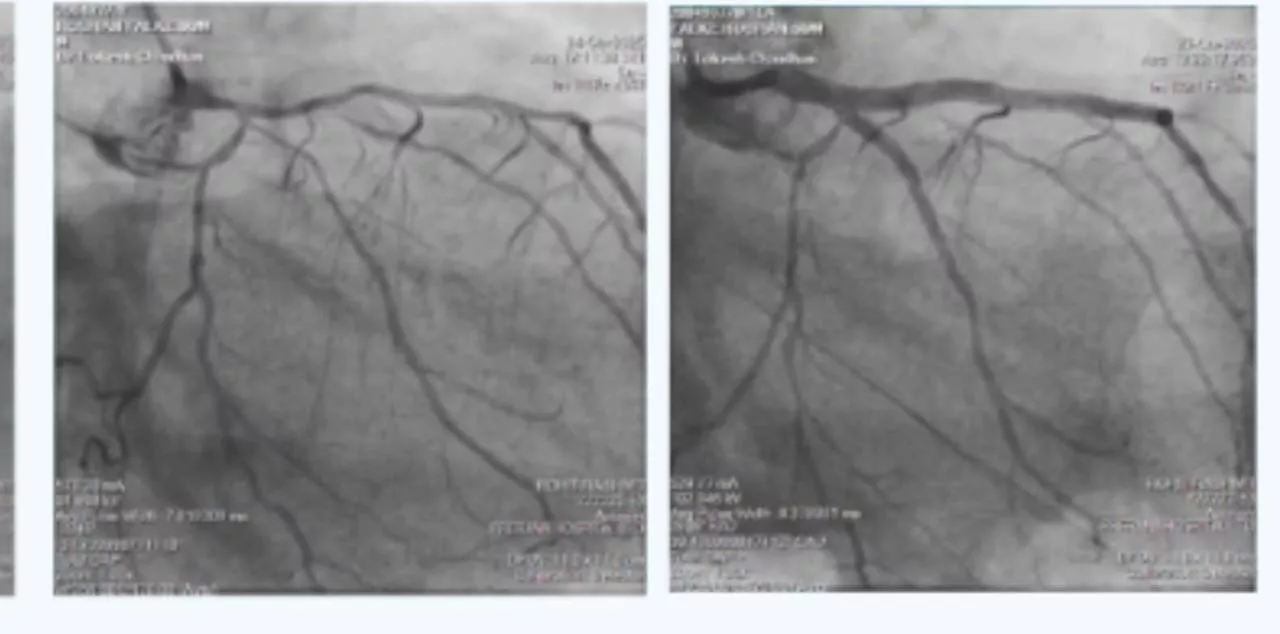
A 68-year-old male, with a known hypertension, developed a dull, aching abdominal pain radiating to the back for 2–3 weeks. On examination, pulsatile swelling was noted in the mid-abdomen. Ultrasound and CT revealed a 5.8 cm infrarenal AAA. Patient underwent EVAR (Endovascular Abdominal Aneurysm Repair) using endurant main body stent graft and Iliac limb extension. The procedure was done under local anesthesia. There were no intraoperative complications and no endoleak on post-op angiogram. The patient was discharged as stable two days post-operative.
Discussion Points
- Timely diagnosis saves lives – this patient could have decompensated any time with a ruptured AAA.
- Minimally invasive EVAR is now a safe, effective alternative to open surgery in most elective cases.
- Early detection in the outpatient setting remains the most critical step — often made by alert family physicians or general practitioners.
What to Look for in Your Practice
- Screen males ≥65 years
- Hypertensives or known atherosclerotic disease
- Smokers
- Family history of AAA
- Coronary artery disease, peripheral vascular disease, or carotid artery disease patients.
Red Flag Symptoms
- Constant or deep abdominal/back pain
- Pulsatile mass on abdominal exam
- Sudden drop in haemoglobin (in known AAA)
- Unexplained syncope or hypotension
Tip: A quick abdominal ultrasound is often enough to detect an AAA.
When to Refer
- AAA size ≥5.0–5.5 cm (even if asymptomatic)
- Any symptomatic AAA (pain, fullness, pressure)
- Incidental finding of AAA on imaging
- Known AAA with growth >0.5 cm/year
EVAR, when performed electively, offers:
- Low perioperative risk
- Short hospital stay (2–3 days)
- Early return to routine
- No large incisions
Follow-Up in This Case
- Single antiplatelet and statin therapy
- Routine imaging surveillance (1 month, 3month, 6 month and then annually)
- Lifestyle advice: low salt diet, no lifting >5 kg for 6 weeks.
Final thoughts
Early detection of AAA lies largely in outpatient practice and family doctors are the first line of defence. Your clinical eye, your palpation skills, and your awareness can change the outcome of a patient’s life.