Abstract
Background:
Pleomorphic adenoma is the most common benign neoplasm of the parotid gland, frequently involving the superficial lobe. Lesions located at the anterior border of the gland pose surgical challenges due to their close relationship with the Stensen’s duct and the facial nerve. Traditional extraoral approaches, though effective, risk visible scarring and injury to vital structures. A transoral approach offers a minimally invasive and cosmetically superior alternative.
Case Presentation:
We report a case of a 38-year-old male presenting with a painless swelling in the left cheek, diagnosed radiologically and cytologically as pleomorphic adenoma arising from the anterior border of the left parotid gland. The lesion was excised via a transoral route with intraoperative DJ stent-assisted identification and preservation of the parotid duct. The postoperative course was uneventful, with complete ductal patency and no facial nerve weakness or sialocele formation.
Conclusion:
The transoral excision technique with duct preservation and stenting represents a safe, function-preserving, and cosmetically excellent method for managing small anterior parotid tumors. This approach minimizes morbidity while maintaining oncologic safety and aesthetic outcomes.
Keywords: Parotid gland · Pleomorphic adenoma · Transoral excision · Stensen’s duct preservation · DJ stent · Facial nerve · Cosmesis
Introduction
Pleomorphic adenoma accounts for approximately 60–70% of benign salivary gland neoplasms, most commonly arising in the parotid gland. Lesions involving the anterior border of the gland are relatively uncommon and may clinically mimic buccal mucosal or accessory parotid tumors due to their anterior and superficial location.
Conventional approaches such as preauricular or Risdon incisions allow adequate exposure but are associated with visible scars and risks to the facial nerve and parotid duct. The transoral approach has emerged as a minimally invasive alternative for anteriorly placed, well-encapsulated lesions. It provides direct access through the oral vestibule, excellent cosmesis, and faster recovery when performed by experienced surgeons.
This report describes a case of anterior border pleomorphic adenoma of the parotid gland successfully excised transorally using DJ stent-assisted duct preservation.
Case Details
Patient Profile
A 38-year-old male, presented with a gradually increasing, painless swelling over the left cheek for several months. There were no complaints of pain, trismus, or facial weakness.
Clinical Examination:
- Pulse: 78/min, BP: 110/70 mmHg, SpO₂: 97% (room air)
- Respiratory System: Clear
- Cardiovascular System: S1 S2 +
- CNS: Conscious and oriented
- Abdomen: Soft, non-tender
Provisional Diagnosis: Pleomorphic adenoma of the anterior border of the left parotid gland.
Preoperative Evaluation
FNAC: Benign pleomorphic adenoma; no evidence of malignancy or inflammation.
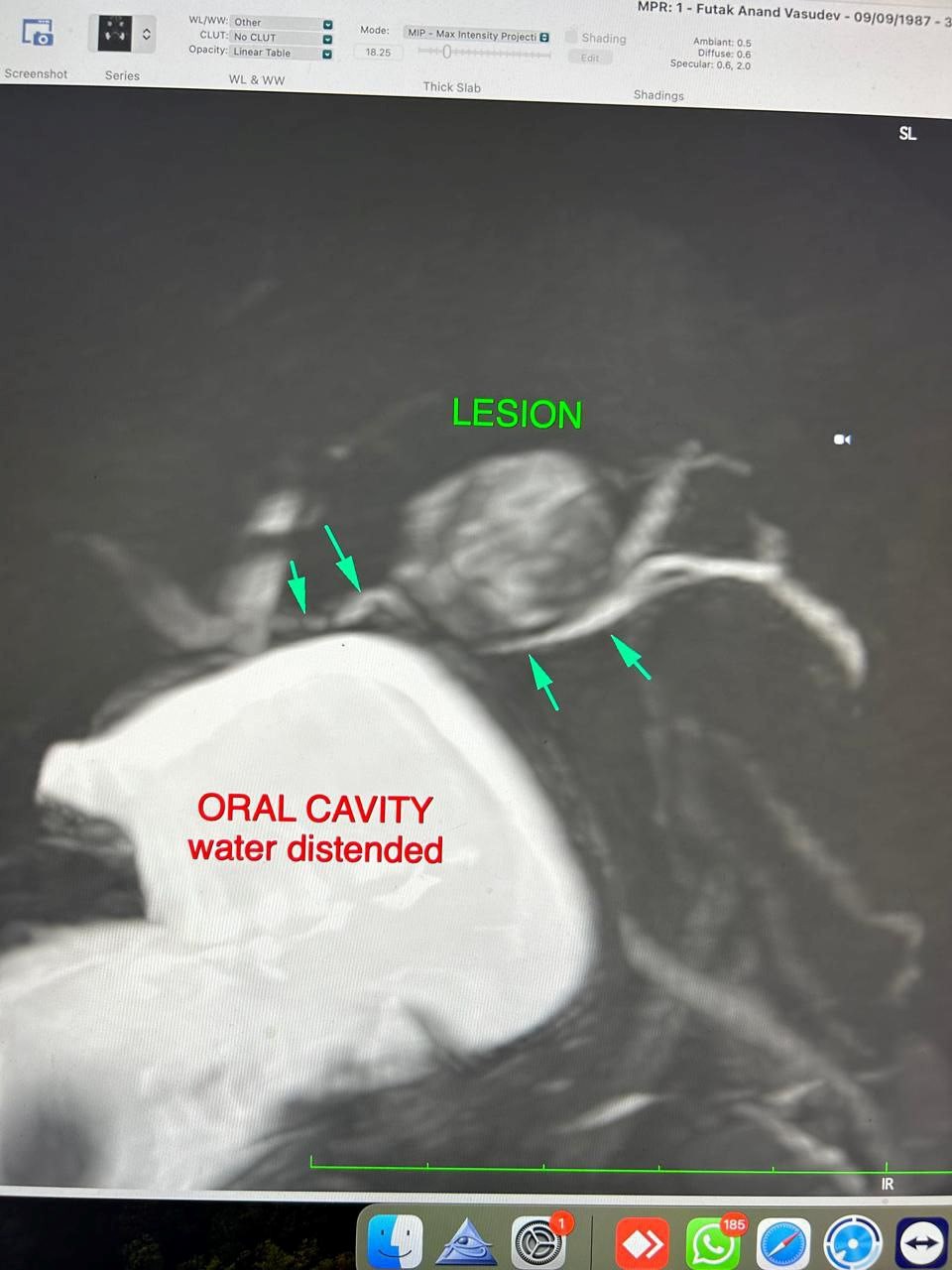
MRI (Neck and Parotid Gland):
A well-defined ovoid lesion measuring 2.0 × 1.6 × 1.3 cm in the left cheek region, hypointense on T1 and heterogeneously hyperintense on T2-weighted images with few cystic foci. The lesion arose exophytically from the anterior portion of the left parotid gland, deep to the buccinator and superficial to the anterior masseter. The parotid duct was displaced inferomedially but remained patent with no proximal dilatation. No deep lobe extension or perineural spread was observed.
Impression: Imaging features consistent with pleomorphic adenoma.

Surgical Procedure
Approach: Transoral intraoral vestibular approach
Operative Findings:
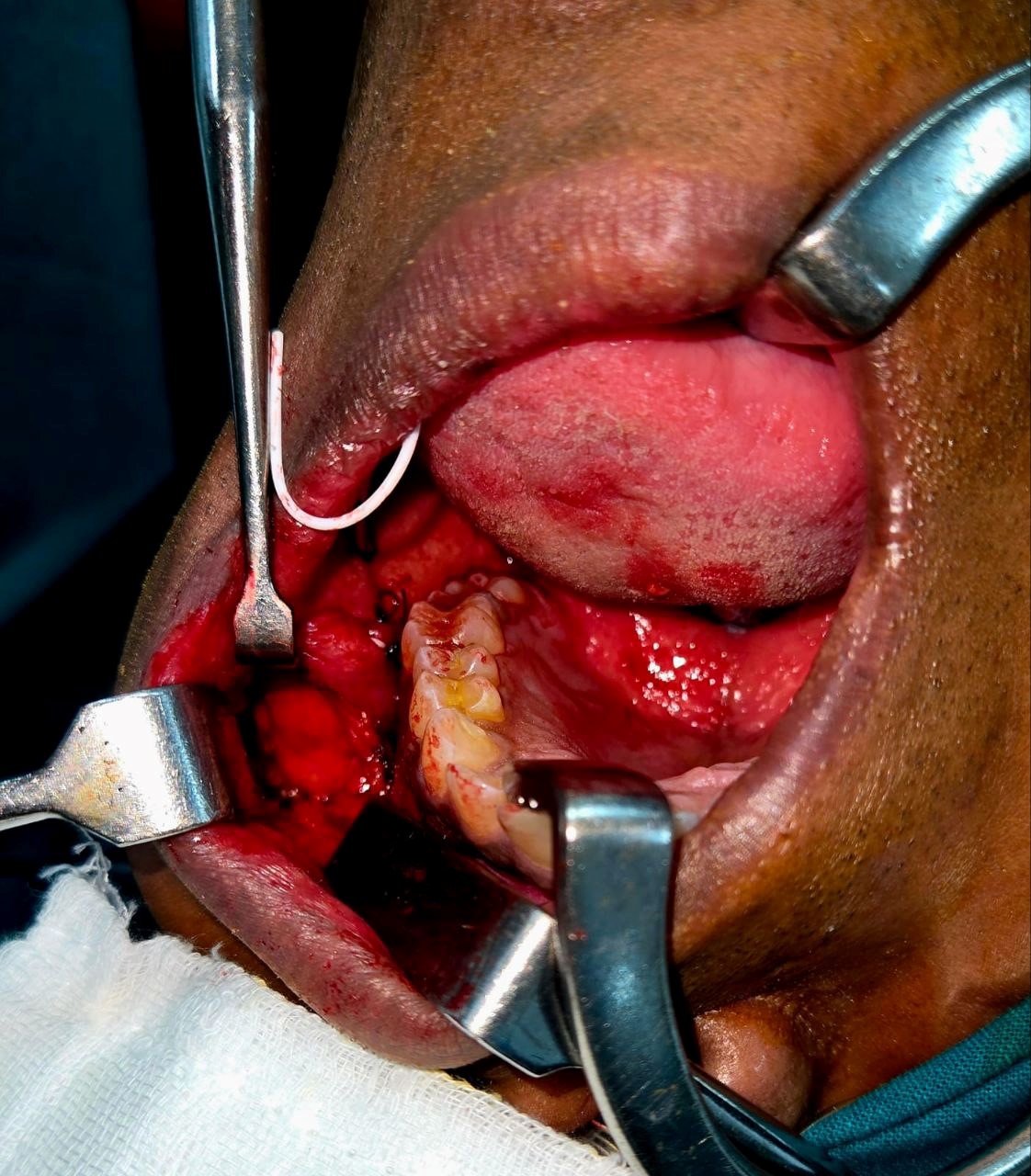
A 2.0 × 1.6 × 1.3 cm well-encapsulated, firm mass was noted at the anterior end of the superficial lobe of the left parotid gland, deep to the buccal fat pad and adjacent to the parotid duct.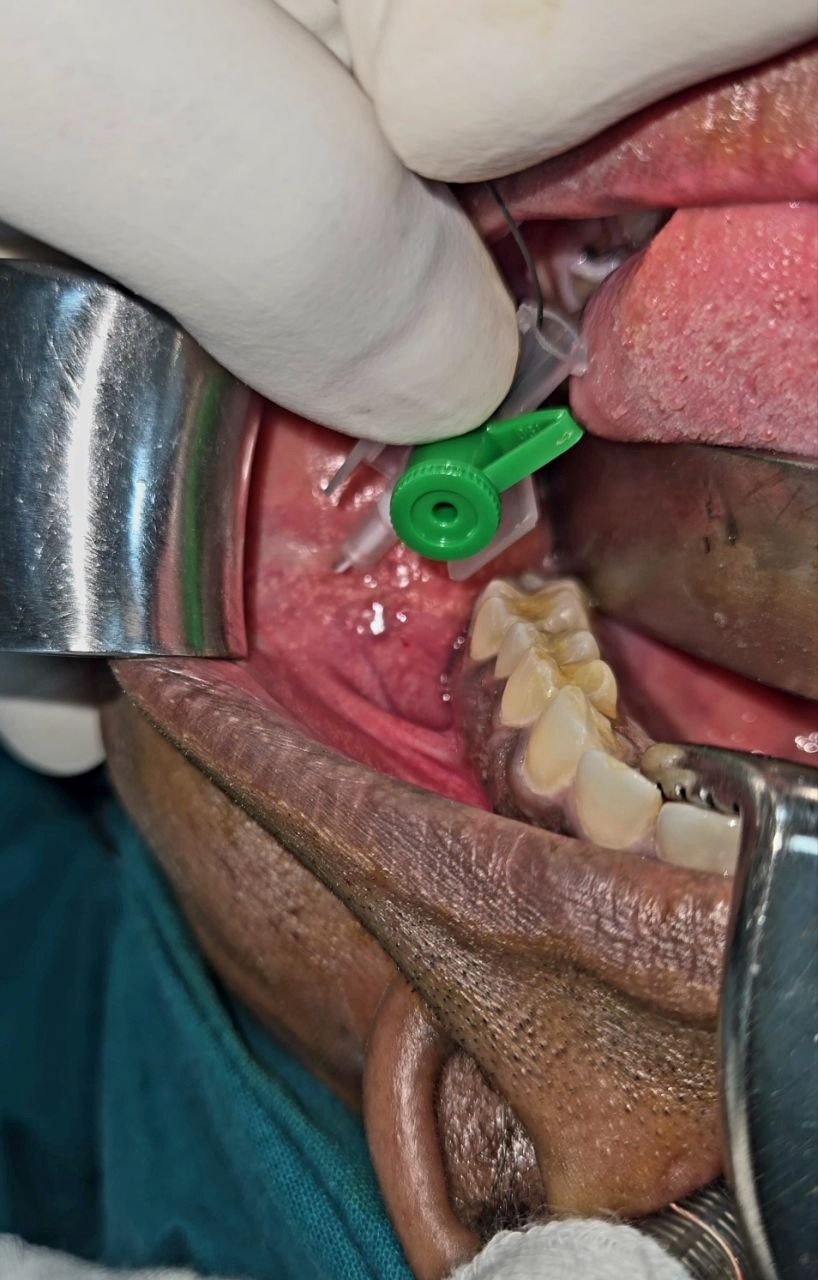
Operative Steps:
- The Stensen’s duct orifice was identified intraorally opposite the upper second molar.
- A guidewire was gently introduced into the duct, and a 3 Fr DJ stent was advanced over it to delineate and protect the duct throughout the procedure.
- Specimen: Encapsulated firm gray-white mass (2.0 × 1.6 × 1.3 cm).
- Estimated Blood Loss: Minimal.
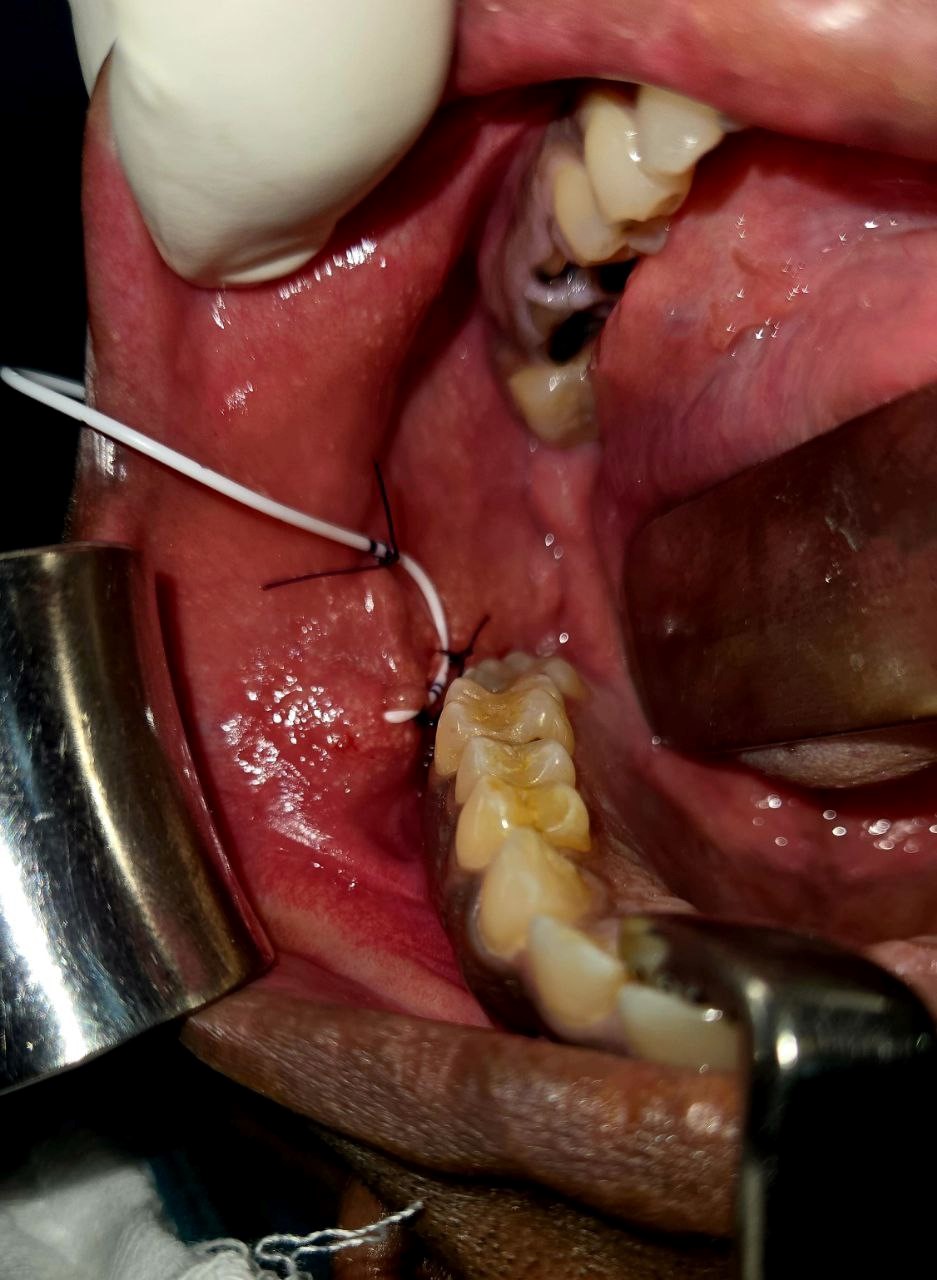
Drain: None. - A horizontal mucosal incision was made in the left upper vestibule, parallel to the course of the duct.
- Peritumoral tumescence with saline-adrenaline solution was injected transcutaneously to facilitate atraumatic dissection.
- Blunt dissection through the buccinator fibers exposed the parotid capsule.
- The encapsulated tumor was dissected circumferentially and excised en bloc without capsular rupture.
- Hemostasis was achieved. Duct integrity was confirmed by expressing saliva through the stent.
- Closure was performed over a Surgicel pack in two layers using 4-0 Vicryl.
Postoperative Course
- The patient tolerated the procedure well. There were no signs of sialocele, ductal leak, infection, or facial weakness. The DJ stent was retained in situ for 7 days to maintain ductal patency and then removed without complication.
- Histopathology: Confirmed Pleomorphic Adenoma, completely excised with intact capsule.
- Condition at Discharge: Stable, tolerating oral intake.
- Follow-up: Advised after 5 days for wound evaluation and stent removal.

Discussion
- Pleomorphic adenoma, though benign, requires complete excision with capsule integrity to prevent recurrence. Anterior parotid tumors are challenging due to their proximity to the Stensen’s duct and risk of iatrogenic injury.
- The transoral route provides direct access for small, anteriorly situated, encapsulated lesions while eliminating external scars. However, intraoperative visualization of the duct is crucial. In this case, DJ stent placement enabled safe identification and continuous assessment of duct patency, preventing inadvertent transection or postoperative stenosis.
- This technique underscores the importance of functional preservation alongside oncologic safety. The patient achieved an excellent cosmetic and functional outcome, with no evidence of recurrence or ductal dysfunction on follow-up.
Conclusion
Transoral excision of anterior border parotid pleomorphic adenoma with DJ stent-assisted duct preservation is a safe, minimally invasive, and cosmetically favorable technique. The method ensures complete tumor removal, maintains ductal function, and avoids external scarring, making it particularly suitable for small, anteriorly located, benign parotid tumors.