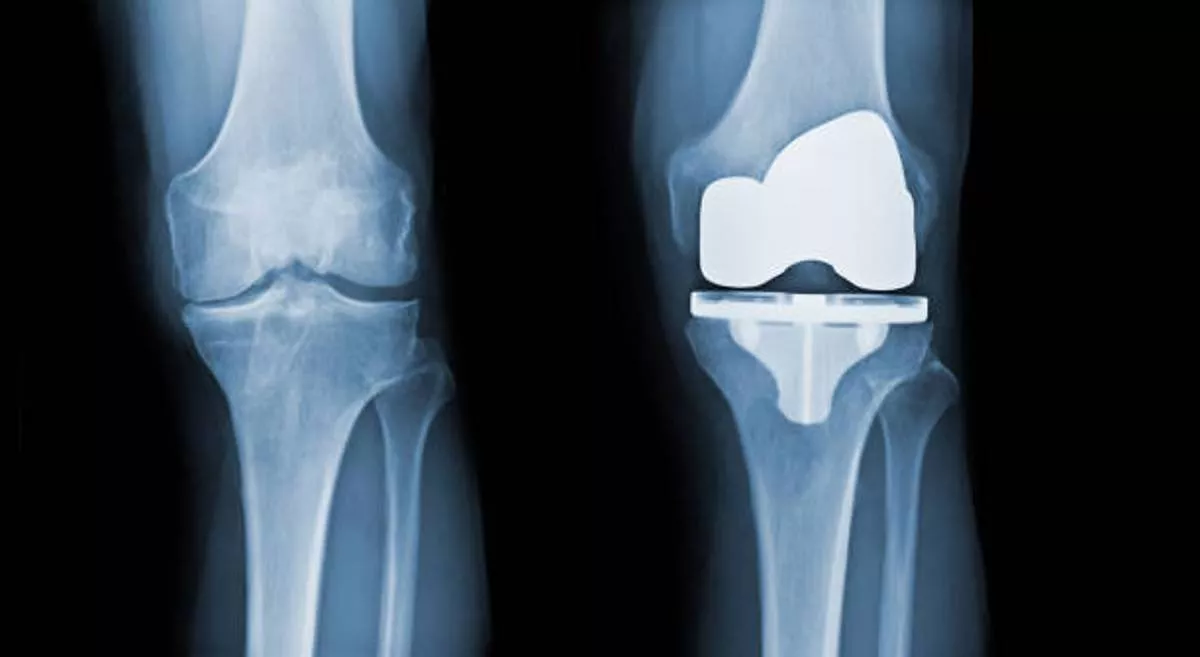
Prosthetic joint infection (PJI) remains a devastating complication after total knee arthroplasty (TKA), It is one of the most common cause of revision for failed knee replacements. Treatment may involve debridement, antibiotic therapy with implant retention (DAIR), and exchange arthroplasty with implant removal as a two-stage procedure or in certain cases as a single-stage revision.
CASE PROFILE:
A 69yr old female came to Aster RV Hospital with pain, swelling, and a discharging sinus from her left knee. She had undergone total knee replacement surgery for her left knee in the year 2018 and 2 years after surgery she underwent multiple wound debridement in view of the infection in the year 2020 and March 2021
DISCUSSION:
It is widely accepted that the successful treatment of infected TKA depends on early correct diagnosis and well-coordinated management by an experienced multidisciplinary team. The clinical suspicion of PJI should always be considered when a TKA becomes painful since pain is still an important factor in >90% of cases. Especially during 0-24 months after primary arthroplasty. For early diagnosis the tests that are currently recommended by most of the infection societies include serum CRP and ESR, synovial fluid CC and PMN%, synovial fluid extended cultures, and should be done for every case when PJI is suspected.
For some difficult-to-diagnose equivocal cases, some additional investigations such as histopathology, synovial AlphaDefensin, next-generation sequencing can also be done. In the presence of a draining sinus, the TKA is always considered infected and staged revision should be scheduled. At the site of aspiration bedside tests can be performed. The leukocyte esterase dipstick test (LET) is a cheap tool allowing for quick decision-making in both preoperative and intraoperative diagnostics. The radiographs in two planes are checked for solid implant fixation (radiolucent lines), presence of osteolytic changes of distal femur/proximal tibia, periarticular ossifications.
INTRA-OPERATIVE FINDINGS AND CHALLENGES:
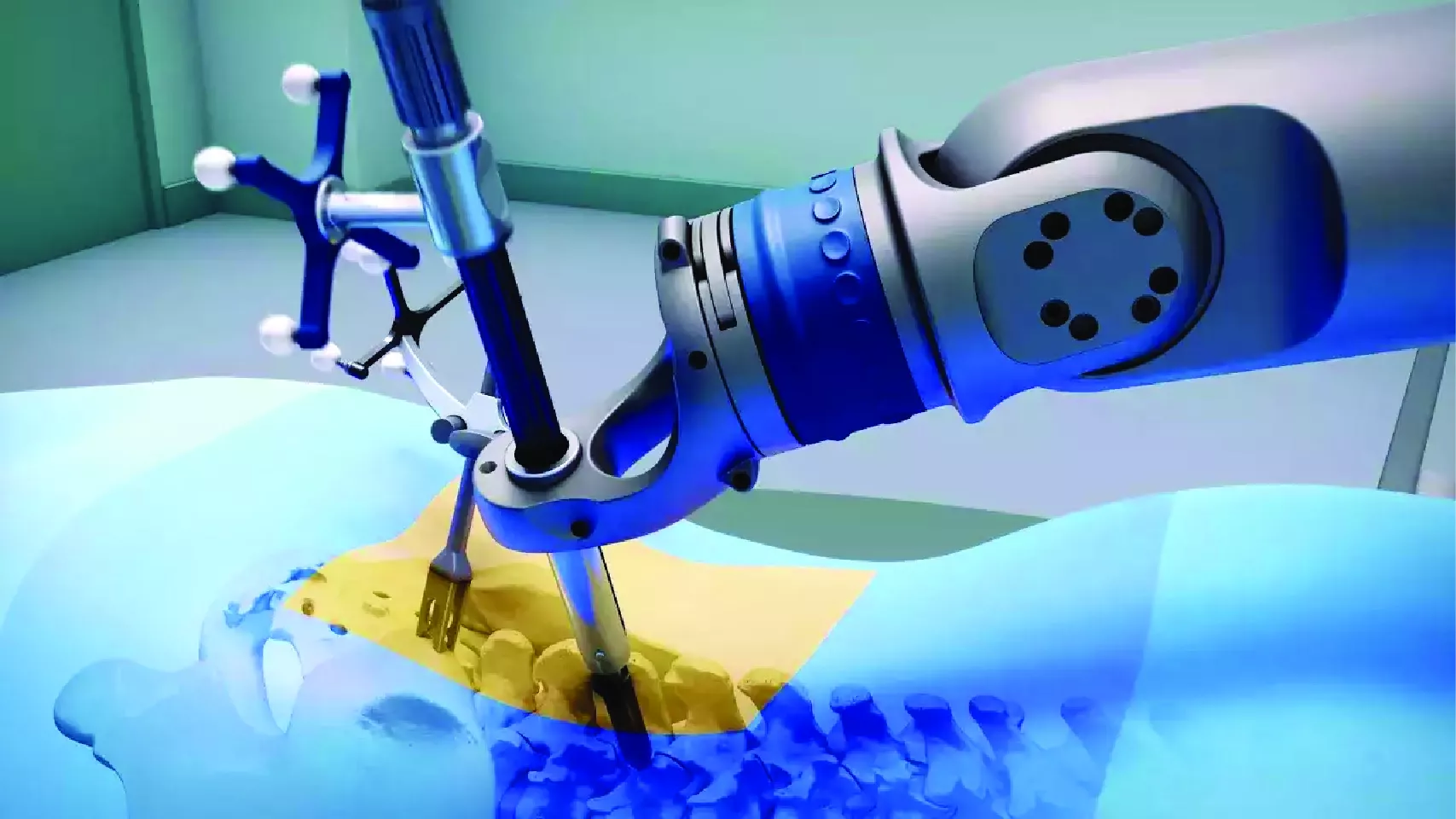
The patient was planned for two-stage revision arthroplasty. During the first operation, aggressive radical soft tissue debridement (figure 3) and removal of all the components of TKR (figure 4 and 5) along with any necrotic infected tissue, including the difficult to access areas such as the posterior capsule of the knee joint is performed. Several samples are taken from different sites for microbiological examination Then, a thorough wash is given with pulsatile jet lavage and antiseptic solution. Under aseptic precautions, a static antibiotic spacer was implanted along with antibiotic beads for local antibiotic delivery. The wound is closed with drain. Targeted antibiotic treatment is continued for 3 weeks. The patient was monitored for CRP, wound, body temperature, and overall clinical picture. After 16 weeks when the patient's CRP is at baseline, the wound is healed, soft tissues are normal, the knee is painless and when the body temperature is normal, stage II revision TKR surgery is performed.
- The cement spacer is removed and aggressive debridement of the bone and soft tissues was performed again, which created a bony defect at the distal femur and it was reconstructed with 4mm medial and 8mm lateral augments.
- Reimplantation of the new prosthesis is performed with stem and 20mm insert. The lateral parapatellar release is done for patellar mal-tracking. The surgical wound is closed with antibiotic beads and drain. Targeted post-op antibiotic therapy as per recommendation from the infection specialist started. Postoperatively CRP, wound healing, general clinical condition monitored.
CONCLUSION:
The infected total knee replacement is a significant challenge for the surgeon and the whole multidisciplinary team, and it is a catastrophic, limb or life-threatening complication for the patient. With early correct diagnosis, adequate classification of the case, and appropriate referral to the centre depending on the complexity of the revision, there is a good chance that most of these patients will receive successful treatment.