Placenta Previa is a serious pregnancy complication that poses considerable risk to both mother and baby. Recognizing its dangers and the importance of timely medical care is crucial to ensuring positive outcomes. With advancements in obstetric management and improved awareness of maternal health, the ability to navigate high-risk conditions like placenta Previa has significantly improved—especially when care is provided at a specialized Gynaecology Hospital in JP Nagar Bangalore equipped to handle complex pregnancies.
What is Placenta Previa?
Placenta Previa occurs when the placenta implants low in the uterus and partially or fully blocks the cervix—the birth canal for a vaginal delivery. This abnormal placement can cause severe bleeding as the pregnancy progresses, particularly in the third trimester. Because of this obstruction, vaginal delivery becomes unsafe, making caesarean section the preferred mode of childbirth in most cases. Although it affects approximately 1 in every 200 to 500 pregnancies, certain factors increase the likelihood of its occurrence. These include a history of previous caesarean sections, multiple pregnancies, prior uterine surgeries, or maternal age over 35.
Why Placenta Previa is Considered High-Risk
The foremost danger associated with placenta Previa is sudden and severe haemorrhage, which can occur without prior symptoms and escalate rapidly. This kind of bleeding endangers the life of both mother and baby, often necessitating emergency medical intervention. Other potential complications include preterm delivery, placental abruption (premature separation), and, in severe cases, the need for a hysterectomy to control bleeding. Given these life-threatening risks, placenta Previa is classified as a high-risk pregnancy, requiring constant monitoring and proactive care from diagnosis to delivery under experienced Gynaecologists in JP Nagar Bangalore.
Multi-Disciplinary Management: A Critical Strategy
Successful management of placenta Previa demands a multi-disciplinary approach. Obstetricians work in tandem with anaesthesiologists, neonatologists, interventional radiologists, and critical care teams to develop a delivery plan that maximizes safety for both mother and child. Early identification through prenatal ultrasound is the cornerstone of care. Once diagnosed, patients are closely monitored, and an elective caesarean section is generally scheduled between 36 and 37 weeks. During delivery, comprehensive protocols—including blood product availability, intensive care readiness, and neonatal support—are put in place to prepare for any emergency
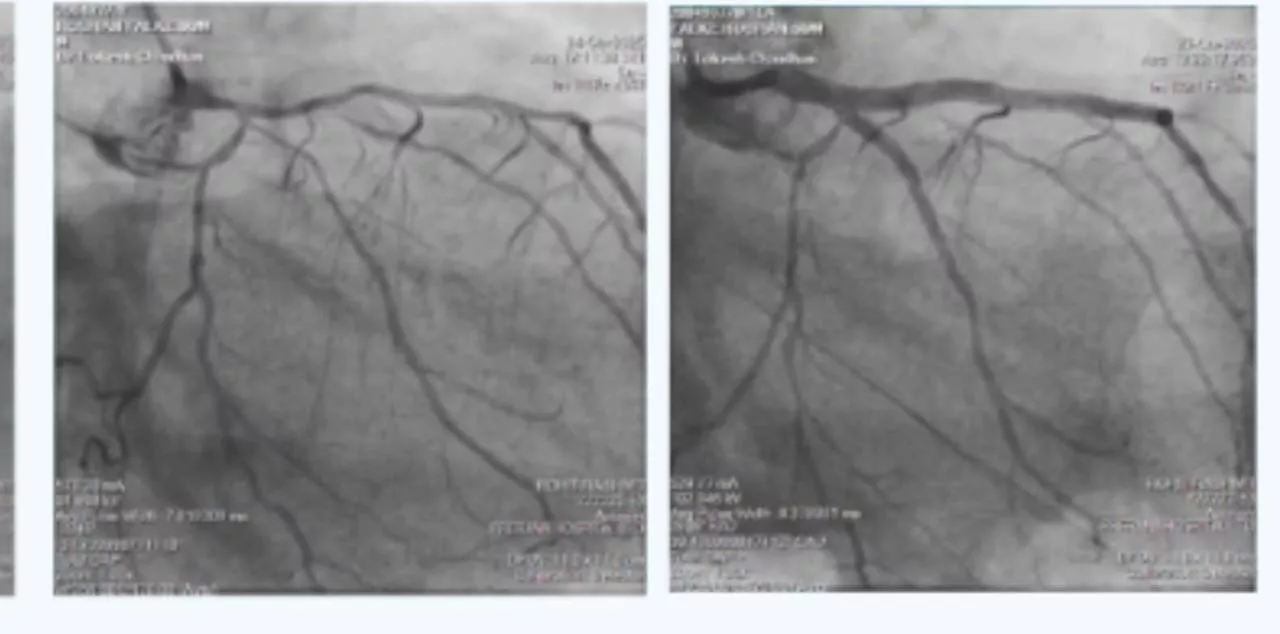
Aster RV Hospital’s Model of Success: Prophylactic Balloon Occlusion in Action
Aster RV Hospital, Bangalore, has emerged as a centre of excellence in the management of high-risk pregnancies, particularly placenta praevia. Since 2021, the hospital's Obstetrics & Gynaecology team has successfully implemented a multidisciplinary protocol that includes prophylactic balloon occlusion (PBO) of the internal iliac arteries during elective caesarean sections for patients with confirmed placenta praevia. In a series of 10 high-risk cases, the hospital combined PBO with lower segment caesarean section (LSCS) under a collaborative plan involving senior obstetricians, interventional radiologists, anaesthetists, intensivists, and a 24/7 on-call blood bank. The results have been remarkable:
- Zero cases of peripartum hysterectomy
- No postoperative blood transfusions
- No balloon-related complications such as thrombosis or ischemia
- Estimated blood loss remained below 1000 mL in all patients
- Short hospital stays of just 2 to 4 days
These outcomes strongly support the efficacy, safety, and reproducibility of PBO as a strategy to mitigate haemorrhagic complications associated with placenta praevia. The results also underscore Aster RV’s capabilities as a tertiary care centre offering advanced interventional procedures and evidence-based obstetric care
The Game-Changer: Internal Iliac Artery Balloon Catheterization
Internal iliac artery balloon catheterization has transformed the way life-threatening placental conditions are managed. This technique involves placing balloon catheters in the internal iliac arteries prior to the caesarean section. Once the baby is delivered, the balloons are inflated to temporarily reduce pelvic blood flow, thereby minimizing intraoperative bleeding. This technique is especially valuable in cases where placenta Previa is complicated by abnormal placental attachment, such as placenta accreta, where the placenta grows too deeply into the uterine wall. In such cases, controlling haemorrhage is paramount to avoid maternal morbidity and preserve fertility.
Promoting Awareness and Preparedness
Placenta Previa underscores the importance of specialized care, preparedness, and public awareness. Regular antenatal visits, access to modern diagnostics, and referral to high-level care centres when needed can make all the difference. Informed patients and vigilant healthcare providers together form the cornerstone of safe delivery practices. In today’s medical landscape, no woman should face life-threatening complications without access to proven solutions. With structured care pathways, expert teams, and technologies like PBO, even complex pregnancies can be managed with confidence and safety