Extracorporeal membrane oxygenation (ECMO) is a life support technique used to support patients with severe respiratory or cardiac failure. The indications for ECMO can vary depending on the patient's condition, but generally include:
- Severe respiratory failure: ECMO may be used for patients who are not responding to mechanical ventilation or other treatments for severe respiratory failure, such as acute respiratory distress syndrome (ARDS), pneumonia, or pulmonary embolism.
- Cardiogenic shock: ECMO may be used for patients with severe heart failure or cardiogenic shock, which is a condition in which the heart is unable to pump enough blood to meet the body's needs.
- Bridge to transplant: ECMO can be used as a bridge to transplant for patients who are waiting for a lung or heart transplant and are critically ill.
- Post-cardiotomy shock: ECMO may be used in patients who develop shock after cardiac surgery, particularly in those with pre-existing cardiac or pulmonary disease.
- Trauma: ECMO may be used for patients with severe lung or heart injury due to trauma.
- Pulmonary hypertension: ECMO may be used for patients with severe pulmonary hypertension, a condition in which the blood pressure in the lungs is elevated and can lead to right heart failure.
- Overdose or poisoning: ECMO may be used in cases of drug overdose or poisoning, in which the patient's lungs or heart may be compromised.
The decision to use ECMO is made by a team of medical professionals, including critical care specialists, pulmonologists, and cardiothoracic surgeons, who will evaluate the patient's condition and determine if the potential benefits of ECMO outweigh the risks. ECMO is a complex and expensive procedure that requires specialized training and expertise, and is typically reserved for patients who are critically ill and not responding to other treatments.
There are two main types of ECMO (extracorporeal membrane oxygenation): venovenous (VV) and venoarterial (VA).
Venovenous (VV) ECMO
Venovenous extracorporeal membrane oxygenation is a type of extracorporeal life support (ECLS) that provides respiratory support to patients with severe respiratory failure. It involves the use of a machine that temporarily takes over the function of the lungs, allowing them to rest and heal.
During VV ECMO, blood is drained from the patient's body through a large catheter (a tube) inserted into a vein, typically in the groin area. The blood is then passed through an oxygenator, which removes carbon dioxide and adds oxygen. The oxygenated blood is then returned to the patient's body through a second catheter, typically inserted into a vein in the neck or chest.
VV ECMO is typically used in patients with severe respiratory failure, such as those with acute respiratory distress syndrome (ARDS), pneumonia, or pulmonary embolism, who are not responding to conventional mechanical ventilation or other treatments. VV ECMO allows the lungs to rest and heal while providing the patient with oxygenated blood.
VV ECMO is a highly invasive and complex procedure that requires specialized equipment and a team of highly trained medical professionals, including pulmonologists, cardiothoracic surgeons, critical care specialists and perfusionists. The patient is closely monitored during VV ECMO, with frequent blood gas analysis to assess oxygen and carbon dioxide levels in the blood.
VV ECMO is associated with a number of risks, including bleeding, infection, clotting, and damage to the blood vessels, among others. However, VV ECMO can be life-saving and may be used as a bridge to recovery or to other treatments, such as lung transplantation.
Venoarterial (VA) ECMO
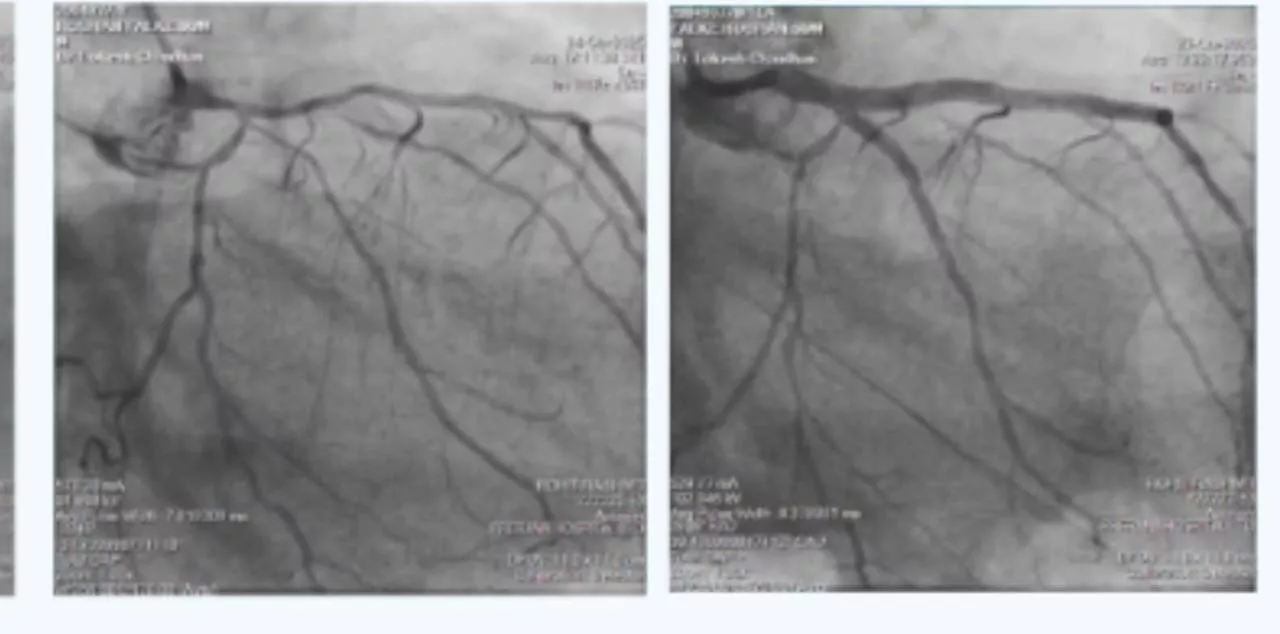
Venoarterial extracorporeal membrane oxygenation is a type of extracorporeal life support (ECLS) that provides both respiratory and cardiac support to patients with severe cardiac and/or respiratory failure. It involves the use of a machine that temporarily takes over the function of the heart and lungs, allowing them to rest and heal.
During VA ECMO, blood is drained from the patient's body through a large catheter (a tube) inserted into a vein, typically in the groin area. The blood is then passed through an oxygenator, which removes carbon dioxide and adds oxygen. The oxygenated blood is then returned to the patient's body through a second catheter, typically inserted into an artery, such as the femoral artery.
VA ECMO is typically used in patients with severe cardiac and/or respiratory failure, such as those with cardiogenic shock, cardiac arrest, or other conditions that can cause severe impairment of both the heart and lungs. VA ECMO provides support to both the heart and lungs, allowing them to rest and heal while providing the patient with oxygenated blood.
VA ECMO is a highly invasive and complex procedure that requires specialized equipment and a team of highly trained medical professionals, including pulmonologist, critical care specialists, cardiothoracic surgeons, and perfusionists. The patient is closely monitored during VA ECMO, with frequent blood gas analysis to assess oxygen and carbon dioxide levels in the blood.
VA ECMO is associated with a number of risks and potential complications, including bleeding, infection, clotting, and damage to the blood vessels, among others. However, VA ECMO can be life-saving and may be used as a bridge to recovery or to other treatments, such as heart transplantation.
ECMO in Covid 19
ECMO (extracorporeal membrane oxygenation) has been used as a treatment for severe cases of COVID-19, particularly in patients with acute respiratory distress syndrome (ARDS) who are not responding to conventional treatments. ECMO can provide respiratory and cardiac support to patients with severe lung damage and low oxygen levels.
The use of ECMO during COVID-19 has been associated with some promising outcomes in select patients, although it is not a suitable treatment for all patients with severe COVID-19. ECMO is a highly invasive and complex procedure that requires specialized equipment and a team of highly trained medical professionals. As a result, it is typically reserved for critically ill patients who have not responded to other treatments.
ECMO is associated with a number of risks and potential complications, including bleeding, infection, and damage to the blood vessels. Patients who receive ECMO during COVID-19 require close monitoring, and the decision to use ECMO is typically made on a case-by-case basis, taking into account the patient's individual clinical condition, overall health, and other factors.
In some cases, ECMO may be used as a bridge to other treatments, such as lung transplantation or recovery. It is important to note that ECMO is not a cure for COVID-19, and patients who receive ECMO may require additional treatment and support after they have been weaned off the machine.
The use of ECMO (extracorporeal membrane oxygenation) has increased in recent times, particularly during the COVID-19 pandemic. ECMO has been used as a treatment for severe respiratory failure in patients with COVID-19 who are not responding to conventional treatments. During the pandemic, there has been a significant increase in the number of patients with severe respiratory failure, particularly those with acute respiratory distress syndrome (ARDS) associated with COVID-19. ECMO has been used in some of these patients as a last resort treatment option, and there have been reports of positive outcomes, including improved survival rates and reduced need for mechanical ventilation.
ECMO (extracorporeal membrane oxygenation) has been associated with good outcomes in certain patients with severe respiratory and/or cardiac failure. The use of ECMO is typically reserved for critically ill patients who have not responded to conventional treatments, and it can be a life-saving intervention in some cases.
One example of a condition where ECMO has been associated with good outcomes is acute respiratory distress syndrome (ARDS), which is a severe lung injury that can be caused by a variety of factors, including infections, trauma, and other conditions. ECMO has been used as a treatment for severe ARDS, and studies have shown that it can improve survival rates and reduce the risk of complications.
ECMO has also been used in patients with severe cardiac failure, such as those with cardiogenic shock or cardiac arrest. In these cases, ECMO can provide temporary support to the heart and circulatory system, allowing the heart to rest and heal. Studies have shown that ECMO can be effective in improving survival rates and reducing the risk of complications in these patients.